Mid-term results after single incision transumbilical laparoscopic sleeve gastrectomy
Introduction
The prevalence of overweight and obesity has been increasing globally. Obesity increases the likelihood of various diseases, particularly heart disease, type 2 diabetes, hypertension, obstructive sleep apnea, asthma, certain types of cancer, and osteoarthritis (1,2). It is a leading preventable cause of death worldwide, with increasing prevalence in adults and children, and authorities view it as one of the most serious public health problems of the 21st century (3). On average, obesity reduces life expectancy by six to seven years (3,4) a BMI of 30-35 kg/m2 reduces life expectancy by two to four years (5), while severe obesity (BMI >40 kg/m2) reduces life expectancy by ten years (5,6).
In Western countries, the Morbid Obesity is defines as: BMI ≥40 kg/m2, or BMI ≥35 kg/m2 with severe obesity-related morbidities. However, Asians are more prone to develop obesity-related disease at a lower BMI than Caucasian, and in Asia-Pacific Region, we define Morbid Obesity according to the guideline from the Consensus Statement from Asia-Pacific Bariatric Surgeons Group in 2005: BMI ≥37 kg/m2, or BMI ≥32 kg/m2 plus Type 2 Diabetes or two obesity-related co-morbidities.
The most effective treatment for obesity is bariatric surgery. Surgery for severe obesity is associated with long-term weight loss, resolution of comorbidities, and decreased overall mortality.
Laparoscopic sleeve gastrectomy (LSG) for treatment of morbid obesity was first described as a part of the more complex operation, biliopancreatic diversion with duodenal switch (BPD/DS). Thereafter, LSG was performed as a first-stage procedure in high-risk patients with a body mass index (BMI) of more than 60 to obtain an initial weight loss with low morbidity and mortality (7).
Recently, LSG has been gaining wide popularity as a stand-alone procedure for the treatment of morbid obesity. The accelerating enthusiasm toward this procedure is driven by its relative simplicity compared with LRYGB and BPD/DS, and its promising early and long term results (8,9).
LSG has shown to provide weight loss comparable to LRYGB and LBPD-DS but with the added advantage of having lesser morbidity and along with resolution of co-morbidities such as diabetes, hypertension, and dyslipidemia (10,11). Lately, we published our 5 years experience in LSG, and the results was encouraging and comparable to LRYGB in terms of weight loss and resolution of co-morbidities (12).
Single-incision laparoscopic surgery (SILS) was first described as early as 1992 by Pelosi et al. performed single-puncture laparoscopic appendectomy and hysterectomy (13). Applications of SILS have expanded rapidly and various procedures including bariatric surgery have been carried out with this technique. The first SILS sleeve gastrectomy was performed by Saber et al. in 2008, thereafter a few reports of SILS-LSG were published with encouraging short-term results (EWL%, resolution of co-morbidities, and complication rate were comparable to that of conventional 5 ports LSG, with the advantage of better cosmetic results, less abdominal pain, and shorter hospital stay) (14-16).
In 2010 we published our preliminary results of SITU laparoscopic bariatric surgery including 6 cases of SITU-LSG and the short term results were quite satisfactory (17). Here, after 3 years of our previous study and with a larger number of patients we want to evaluate the safety, feasibility, and efficacy of SITU-LSG, and show the mid-term results regarding EWL%, resolution of co-morbidities and cosmetic outcome.
Materials and methods
Between November 2008 and November 2012, 51 morbidly obese patients had undergone SITU-LSG. The patients were fully informed about the procedures, and informed consent was obtained from them. The indications for SITU-LSG were consistent with Asian Pacific Bariatric Surgery Society guidelines for Bariatric Surgery (2005):
- Age between 18-65 years;
- BMI ≥32 kg/m2 with obesity-related co-morbidities or ≥37 kg/m2 irrespective of co-morbidities.
Exclusion criteria in our study were:
- Patients with BMI ≥50 kg/m2;
- Body height ≥180 cm;
- Severe GERD or Barrett’s disease;
- History of alcohol or drugs abuse.
Each patient was preoperatively screened and evaluated by a multidisciplinary bariatric team. Preoperative pan endoscopy (OGD scopy) was routinely performed to test for Helicobacter pylori, and screen for neoplasms or peptic ulcers. Patients were admitted one day prior to surgery and were prescribed liquid diet for a day. A proton pump inhibitor (PPI) and a single dose of intravenous antibiotic (Cefazolin) were intravenously administered 1 hour before surgery. The same operative technique and perioperative protocol was used in all patients. Data was prospectively collected and retrospectively analyzed. This study was conducted with the approval of E-Da Hospital institutional review board.
Operative technique
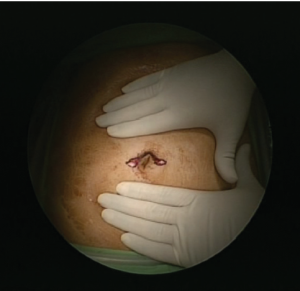
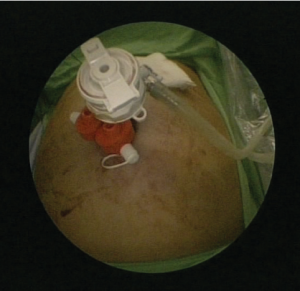
The patient was placed in the supine position with the arms extended laterally. An anesthesiologist induced general anesthesia and performed endotracheal intubation. For most operations, the surgeon stood on the right side of the patient and the assistant on the left. A 4-cm-long omega-shaped incision was made around the upper half of the umbilicus (Figure 1). The incision was deepened to the linea alba after dissecting the subcutaneous fat, and a 15-mm Versaport plus V2 trocar (Covidien) was inserted after establishing pneumoperitoneum, produced by carbon dioxide insufflation at a pressure of 15 mmHg. A 5-mm-long, rigid, 30° video laparoscope was then inserted. Under direct visualization, two 5 mm Versaport plus V2 trocars (Covidien) were inserted through both arms of the omega incision (Figure 2). We then inserted the liver-suspension tape (LST) into the peritoneal cavity. We used our novel previously published technique in liver suspension (18). One needle was placed in a needle holder, inserted into the lateral edge of the left liver lobe, and brought out through the abdominal wall in the left upper quadrant; the other needle was inserted into the left liver lobe near the falciform ligament and then brought out through the abdominal wall in the right upper quadrant. The liver was then retracted to an appropriate position, and the sutures were suspended with clamps (18). After achieving the appropriate liver traction, we commenced the surgical procedure.
In the SITU-LSG procedure, devascularization of the greater curvature was started 4 cm away from the pylorus and continued till the angle of His, using the 5 mm Ligasure (Tyco, New Haven, CT, USA). The posterior adhesions were taken down to prevent redundant posterior wall of the sleeve, and the angle of His was completely mobilized with exposure of the left crus of the diaphragm to facilitate complete resection of the gastric fundus.
A 36 Fr orogastric tube was inserted along the lesser curvature into the pylorus and retained as a stent for vertical gastrectomy using Endo GIA. Stapling under the guidance of calibration helps to prevent stenosis, and provides a uniform shape of the sleeve. We used a green load at a distance of 4 cm from the pylorus for the first firing and subsequently blue loads were used. Care must be taken when the first stapler is fired, as a distance of about 3 cm from the incisura angularis should be left to prevent stenosis. After the completion of the main operative procedure, the LST was removed and hemostasis was achieved by cauterization. All trocars were removed and the surgical specimens were extracted via the 15-mm umbilical defect through which a trocar had been inserted. All the fascial defects were closed individually with 2-0 Vicryl sutures. Subsequently, the wound was closed and dressing applied. Patients were transferred to the postoperative recovery room and then to the ward, provided their immediate postoperative course was uneventful. They were permitted to drink water and discharged early if they did not develop any complications.
Results
51 patients underwent SITU-LSG. They were 13 males and 38 females. The mean age was 31±7.7 years (range, 18-50 years), and the mean preoperative body mass index (BMI) was 36.32+2.89 kg/m2 (range, 32.16-45.67 kg/m2). Pre-operative comorbidities are shown in Table 1.
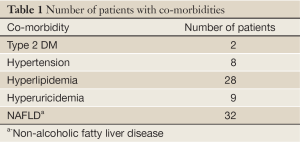
Full Table
The procedure was successfully performed in all patients without inserting additional trocars, or conversion to conventional 5 ports or open surgery. The mean operative time was 72±27.91 minutes (range, 30-170 minutes). No intraoperative complications occurred. The mean hospital stay was 2±0.84 days (range, 1-5 days). No mortality, leak, stricture, or wound infection occurred. One patient developed wound seroma, easily treated with aspiration. Another patient required re-admission 2 weeks after surgery because of severe vomiting and dehydration, however medical management with IV fluids and PPI was successful and the patient discharged 2 days later. No incisional hernia occurred during 2 years of follow up. The excess weight loss (EWL%) was 73.86±7.511% (range, 48.43-102.95%) and 76.12±17.54% (range, 43.35-103.16%) at 1 and 2 years after surgery, respectively. Resolution of co-morbidities at 2 years after surgery was as follows: Type 2 DM (1 patient), hypertension (4 patients), hyperlipidemia (6 patients), hyperuricaemia (9 patients), hyperlipidemia (6 patients), NAFLD (9 patients). More details about resolution of co-morbidities are shown in Table 2. Patients were satisfied with the cosmetic results.
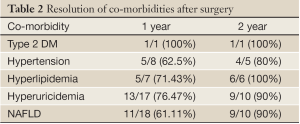
Full Table
Discussion
The evolution of MIS provides an opportunity to successfully perform a variety of surgical procedures through a single small incision on the abdominal wall using a technique called SILS. The application of this new technique in bariatric surgery has technical difficulties due to excessive visceral fat, huge fatty liver and difficulty of the SILS procedure itself in morbidly obese patients.
To gain popularity and acceptance in the field of bariatric surgery, single incision bariatric surgery should prove its feasibility, safety, efficacy and should at least lead to similar results to those of conventional laparoscopic bariatric surgery. This study included patients with BMI between 32 and 45 kg/m2. We followed the Asian Pacific Bariatric Surgery Society guidelines for Bariatric Surgery (2005) to define morbid obesity and include patients in our study. Saber et al. and Pourcher et al. used the National Institutes of Health consensus criteria for inclusion (BMI more than 35 with comorbidities, or more than 40 without comorbidities) (14,19). The cut-offs for obesity definition in Asian people are lower because obesity-related co- morbidities are more likely to occur with lower BMI values in these ethnicity.
We excluded patients with BMI >50 kg/m2, because those patients will have excessive loose skin after losing weight and will mostly ask for abdominoplasty later. Also tall patients with body height more than 180 cm were excluded from our study, because even with the use of long instruments, it is still difficult to reach the angle of His, and adequate dissection around the left crus and complete resection of the fundus are difficult. We use the umbilicus as the site of the incision, because it can hide the scar, so that the cosmetic results would be better. Most previous studies used the same site and reported good cosmetic results (14,16).
The main drawback to performing advanced laparoscopic surgery via the transumbilical approach is the crowding of instruments in a small incision and the small degree of instrument triangulation. We used 3 trocars (one 15 mm and two 5 mm) through a 4 cm incision (in the first 6 cases we used a 6 cm incision). Saber et al. used 3 trocars through an umbilical incision (14,15), while Lakdawala et al., Prourcher et al., and S. Delgado et al. used single port device introduced through the umbilicus (16,19,20). We found that using 3 trocars -SITU-LSG technique can create some degree of triangulation and, facilitate the movement of instruments inside and outside the abdomen, and reduce its clashing.
The mean operative time in our SITU-LSG series (72 minutes) was comparable to that of conventional LSG in the other series, and to that of our recently published study about LSG (60.63 minutes). Lakdawala et al. also reported a median operative time of 50 minutes in his series (N=50 patients), while the mean time was 79.2, and 128 minutes in S. Delgado et al. (20 patients) and P. Gentileschi et al. (8 patients) series, respectively (16,20,21).
All operations in our study were successful and completely done without intraoperative complications and without the need for additional trocars or the conversion to conventional LSG procedure. We feel that our novel technique in liver suspension (LST) eliminated the need to use additional trocar for liver retraction. In Lakdawala et al. study, all the operations were completed without conversion to conventional LSG or adding additional trocars (16). S. Dalgado et al. used additional epigastric 2-or 3-mm miniport for liver retraction in all patients in his series (N=20), and 1 patient required conversion to conventional LSG (20). In Pourcher et al. series (N=60 patients), 10 patients required a second trocar and 3 patients 2 additional trocars (19).
The mean length of hospital stay in our series was 2 days, without major complications or mortality. Only one patient developed wound seroma, easily managed with aspiration. In his series, Lakdawala et al. reported a median length of hospital stay of 2 days, without complications or mortality (16), while Pourcher et al. reported a median length of 4 days, with 1 patient developed leak from the upper gastric zone, successfully treated by a covered endoscopic prosthesis (19). S. Delgado et al. reported postoperative hemoperitoneum occurred in 2 patients, and required early reoperation 1 day after surgery (20). To reduce complication rate and to safely perform SITU-LSG, adequate experience in conventional LSG should be available.
Although it gives better cosmetic results when compared to conventional LSG, SITU-LSG should prove its efficacy in terms of weight loss, and resolution of co-morbidities to be accepted as a bariatric procedure.
In our series, SITU-LSG was quite effective, with a mean EWL% of 73.86% and 76.12%, 1 and 2 years after surgery, respectively. These mid-term results are comparable to that of our recently published study (12) and other studies on conventional LSG. To the best of our knowledge, this is the first study that gives 1 and 2 results after SITU-LSG.
Conclusions
SITU-LSG is safe, feasible and reproducible procedure. No important wound complications occurred during a follow up of 2 years and patients were satisfied with the cosmetic results of the procedure. The mid-term results regarding weight loss, and resolution of comorbidities are encouraging, and comparable to that of conventional LSG. Based on these results, this procedure can be recommended for morbidly obese patients with BMI less than 50 kg/m2 and body height less than 180 cm who seek better cosmetic results.
Acknowledgements
The authors would like to thank the entire staff of the Bariatric surgery center, E-da Hospital, for their help in obtaining the necessary information required for this paper and especially thank Miss Ivy Huang, the case manager, for helping with the data retrieval.
Disclosure: The authors declare no conflict of interest.
References
- Haslam DW, James WP. Obesity. Lancet 2005;366:1197-209.
- Poulain M, Doucet M, Major GC, et al. The effect of obesity on chronic respiratory diseases: pathophysiology and therapeutic strategies. CMAJ 2006;174:1293-9.
- Barness LA, Opitz JM, Gilbert-Barness E. Obesity: genetic, molecular, and environmental aspects. Am J Med Genet A 2007;143A:3016-34.
- Peeters A, Barendregt JJ, Willekens F, et al. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med 2003;138:24-32.
- Prospective Studies Collaboration, Whitlock G, Lewington S, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373:1083-96.
- Colquitt JL, Picot J, Loveman E, et al. Surgery for obesity. Cochrane Database Syst Rev 2009;(2):CD003641.
- Regan JP, Inabnet WB, Gagner M, et al. Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg 2003;13:861-4.
- Baltasar A, Serra C, Pérez N, et al. Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg 2005;15:1124-8.
- Akkary E, Duffy A, Bell R. Deciphering the sleeve: technique, indications, efficacy, and safety of sleeve gastrectomy. Obes Surg 2008;18:1323-9.
- Trelles N, Gagner M. Updated review of sleeve gastrectomy. The Open Gastroenterol J 2008;2:41-9.
- Vidal J, Ibarzabal A, Romero F, et al. Type 2 diabetes mellitus and the metabolic syndrome following sleeve gastrectomy in severely obese subjects. Obes Surg 2008;18:1077-82.
- Zachariah SK, Chang PC, Ooi AS, et al. Laparoscopic Sleeve Gastrectomy for Morbid Obesity: 5 Years Experience from an Asian Center of Excellence. Obes Surg 2013. [Epub ahead of print].
- Pelosi MA, Pelosi MA 3rd. Laparoscopic supracervical hysterectomy using a single-umbilical puncture (mini-laparoscopy). J Reprod Med 1992;37:777-84.
- Saber AA, Elgamal MH, Itawi EA, et al. Single incision laparoscopic sleeve gastrectomy (SILS): a novel technique. Obes Surg 2008;18:1338-42.
- Saber AA, El-Ghazaly TH, Minnick DB. Single port access transumbilical laparoscopic Roux-en-Y gastric bypass using the SILS Port: first reported case. Surg Innov 2009;16:343-7.
- Lakdawala MA, Muda NH, Goel S, et al. Single-incision sleeve gastrectomy versus conventional laparoscopic sleeve gastrectomy--a randomised pilot study. Obes Surg 2011;21:1664-70.
- Huang CK, Tsai JC, Lo CH, et al. Preliminary surgical results of single-incision transumbilical laparoscopic bariatric surgery. Obes Surg 2011;21:391-6.
- Huang CK, Lo CH, Asim S, et al. A novel technique for liver retraction in laparoscopic bariatric surgery. Obes Surg 2011;21:676-9.
- Pourcher G, Di Giuro G, Lafosse T, et al. Routine single-port sleeve gastrectomy: a study of 60 consecutive patients. Surg Obes Relat Dis 2012. [Epub ahead of print].
- Delgado S, Ibarzabal A, Adelsdorfer C, et al. Transumbilical single-port sleeve gastrectomy: initial experience and comparative study. Surg Endosc 2012;26:1247-53.
- Gentileschi P, Camperchioli I, Benavoli D, et al. Laparoscopic single-port sleeve gastrectomy for morbid obesity: preliminary series. Surg Obes Relat Dis 2010;6:665-9.