An unusual pancreatic mass: a case report and literature review
Case presentation
A 60-year-old female presented with jaw pain for one month. She also had abdominal pain associated with nausea and vomiting, yellowing of eyes, poor oral intake and 20 pound weight loss over two months. She was found to have abnormal liver function tests with total bilirubin 13.5 mg/dL (normal 0-1 mg/dL), direct bilirubin 9.7 mg/dL (normal 0-0.3 mg/dL), AST 463 U/L (normal 15-37 U/L), ALT 401 U/L (normal 30-65 U/L) and alkaline phosphatase 594 U/L (normal 50-136 U/L).
Diagnosis
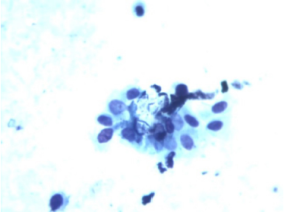
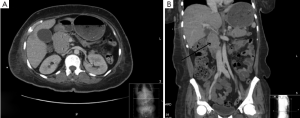
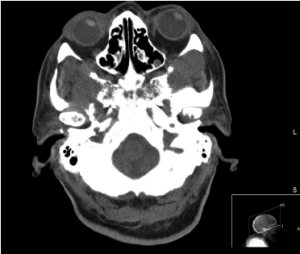
Computed tomography (CT) abdomen with contrast showed a 3.5 cm pancreatic head mass (Figure 1A,B). Endoscopic retrograde cholangiopancreatography (ERCP) revealed narrowing of the lower one third of the common bile duct. Fine needle aspiration cytology (FNAC) of the pancreatic mass showed atypical poorly differentiated cells (Figure 2). Immunohistochemical staining was negative for pan cytokeratin (CK) and CK7 but diffusely positive for lambda light chain and CD138. This pattern was suggestive of plasmacytoma. Further workup to rule out underlying multiple myeloma was conducted. Bone marrow biopsy showed hypercellular marrow with sheets of plasma cells. Flow cytometry revealed a cytoplasmic lambda light chain restricted plasma cell population expressing CD38, CD138 and CD117. CT Face and Mandible showed diffuse permeative infiltration of calvaria and facial bones compatible with metastatic disease (Figure 3). Skeletal survey revealed lytic lesions on the calvarium, left calvicle, bilateral humerus, scapulae, pelvis and right femur.
Additional laboratory testing showed normochromic normocytic anemia, thrombocytopenia, elevated creatinine of 2.1 mg/dL (normal 0.6-1.3 mg/dL) and normal calcium levels. Serum immunoglobulin free kappa light chain 2.04 mg/L (normal 3.3-19.4 mg/L), free lambda 3,600 mg/L (normal 5.71-26.3 mg/L) and kappa/lambda ratio of 0.0006. Beta 2 microglobulin was elevated at 8.18 mg/L. Based on these parameters she was diagnosed with Multiple Myeloma International Staging System (ISS) Stage III.
Management
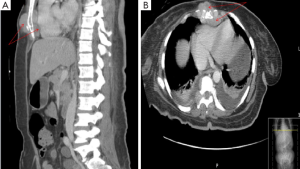
ERCP guided stenting of the biliary tree was unsuccessful. Hence a percutaneous transhepatic cholangiography (PTC) drain was placed to relieve the biliary obstruction. She was started on zoledronate. Due to her poor performance status and extensive disease she was considered a poor candidate for external beam radiation to the pancreatic mass. She was started on multi-agent chemotherapy with bortezomib, cyclophosphamide and dexamethasone. However, her disease course was complicated by multiple episodes of sepsis due to cholangitis and rapidly progressive myeloma. CT Brain showed multiple lobulated masses involving facial bones, calvarium and inferior left temporal lobe. Chest CT showed bilateral large pleural effusions and multiple soft tissue masses adjacent to the lower thoracic vertebral bodies. There was a mass like lesion around the lower sternum causing mass effect upon the anterior wall of right ventricle (Figure 4A,B). She eventually developed multi-organ failure to which she succumbed.
Discussion
Multiple myeloma is a malignant proliferation of a single clone of plasma cells producing a monoclonal immunoglobulin. It represents 10% of hematologic and 1% of overall malignancies in the United States (1). The annual incidence in the US is approximately four to five per 100,000. It is a disease of older adults in the 6th and 7th decades with median age at diagnosis of 66 years (2,3). The clonal proliferation occurs predominantly in the bone marrow causing bone pain, punched out lytic lesions, anemia and hypercalcemia. Production of excessive monoclonal immunoglobulins leads to renal failure.
Plasmacytomas are discrete masses of neoplastic plasma cells. They may be osseous or extramedullary. Extramedullary plasmacytomas are uncommon and represent 5% of all plasma cell tumors (4). Their median age of presentation is 55 years (10 years younger than patients with multiple myeloma) (5). There is male predominance with three-fourths being male (5). Plasmacytomas may be primary or secondary (5). Primary plasmacytomas occur as solitary masses without bone marrow involvement and secondary as part of multiple myeloma. Secondary plasmacytomas are seen in approximately 7% of patients with Multiple myeloma at the time of diagnosis and an additional 6% of patients will develop it later in the disease course (6,7). The upper respiratory tract (nasal fossae, oronasopharynx and paranasal sinuses) is the most common site (80%) of extramedullary plasmacytomas (8). Other sites involved are gastrointestinal tract in about 10% of cases (most commonly the stomach) (9), reticuloendothelial system (liver, spleen and lymph nodes), pancreas, breast, thyroid, lungs, skin and testicles.
Infiltration of the pancreas by the myeloma cells is rare with an incidence rate of 2.3% based on autopsy studies (10). Most common clinical features of pancreatic plasmacytomas are abdominal pain and obstructive jaundice due to obstruction of the biliary tree. Pancreatic plasmacytoma can involve the head (most common) (11), body, tail or cause diffuse involvement. Diagnosis of an extramedullary plasmacytoma depends on finding a mass of monoclonal plasma cells outside the bone marrow. Immunohistochemistry and flow cytometry aid in confirming the monoclonality of plasma cells.
High resolution dual phase (arterial and portal) contrast-enhanced CT has become the primary modality of choice in the evaluation of pancreatic malignancies (12). The CT appearance of pancreatic plasmacytoma is classically described as a focal multilobulated hypodense mass with clear demarcation from the surrounding normal pancreatic parenchyma and with homogeneous intravenous contrast enhancement (13). However, these findings are nonspecific and at times may be difficult to differentiate from other pancreatic tumors, especially those which show enhancement with intravenous contrast such as endocrine cell tumors (islet cell tumors), acinar cell neoplasms, lymphomas and metastases thus necessitating a tissue biopsy for confirmation of the actual diagnosis (14).
CT guided biopsy is, however, associated with a few risks including seeding of malignant cells through the needle track and formation of multiple secondary extramedullary plasmacytomas.
Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) has emerged as a possible diagnostic tool approaching the sensitivity of a helical CT and may also provide adequate material for flow cytometry analysis (15). For diagnosing pancreatic solid masses, EUS-FNA was reported to have a sensitivity of 78-95%, a specificity of 75-100%, a positive predictive value of 98-100%, a negative predictive value of 46-80%, and an accuracy of 78-95% (16). It has been difficult to establish its sensitivity and specificity for pancreatic plasmacytomas per se due to the rarity of the disease.
Abdominal ultrasound is a good initial screening test for patients presenting with obstructive jaundice to rule out other etiologies. However the pancreas is often obscured by overlying gas and lesions less than 3 cm may be missed (17). Magnetic resonance imaging (MRI) has been less studied for evaluation of pancreatic lesions. However some authors suggest that this modality may be better in demonstrating pancreatic infiltration than CT. Positron emission tomography/computed tomography (PET/CT) may help in diagnosing asymptomatic extramedullary plasmacytomas at any site including the pancreas in patients with known multiple myeloma but their definitive role is yet to be established (18).
Treatment for extramedullary plasmacytomas with or without underlying multiple myeloma involves combination of local radiation, surgery and combination chemotherapy. For tumors occupying the head and neck of pancreas, local radiation is the treatment of choice since these tumors are highly radiosensitive. Local control rates ranging from 80-100% have been reported (19). Tumors involving tail of the pancreas can be managed by distal pancreatectomy in good surgical candidates. For diffuse involvement, complete surgical resection should be considered. For patients with positive surgical margins, tumors greater than 5 cm or high grade disease, adjuvant chemotherapy should be used (19). A recent pilot study by Nadia et al. (20) showed that the combination of helical tomotherapy with concurrent molecular targeted therapy with lenalidomide or bortezomib, in patients with solitary plasmacytoma, was able to produce a significant response both clinically and radiologically. Helical tomotherapy delivers highly conformal irradiation which combined with systemic targeted therapy has a better response rate with low toxicity (20). Extramedullary plasmacytomas have a high rate of progression to multiple myeloma. In case of primary progression or response followed by progression, combination chemotherapy with bortezomib (proteasome inhibitor), thalidomide, lenalidomide, doxorubicin or cyclophosphamide along with dexamethasone may be used in varying combinations (21). This may be followed by hematopoietic stem cell transplant (SCT) in suitable candidates. SCT may be single autologous SCT, a tandem SCT (a planned second course of high dose of therapy and SCT within six months of the first) or an allogeneic SCT (either performed after prior myeloablative therapy or non myeloablative therapy) (21). Primary therapy for nontransplant candidates includes Melphalan along with the above mentioned regimens. Bortezomib based regimens are useful in patients with renal failure and adverse cytogenetic features like t[4;14] or del[17p]. However, they are associated with increased incidence of herpes zoster and peripheral neuropathy. Alternative regimens include carfilzomib, lenalidomide and dexamethasone or liposomal doxorubicin, vincristine and dexamethasone. Drugs used for maintenance therapy include bortezomib, lenalidomide or thalidomide. Adjunctive treatments include treatment with bisphosphonates for all patients on treatment for symptomatic myeloma and low dose radiation therapy for palliative treatment of bone pain, impending pathologic fracture or impending spinal cord compression. Hypercalcemia may be treated with hydration and furosemide, bisphosphonates, steroids and calcitonin. Plasmapheresis is required for symptomatic hyperviscosity (21).
In conclusion, our case was unusual because pancreatic plasmacytoma as initial presentation of multiple myeloma is rare. Also fine needle aspiration cytology showed atypical poorly differentiated cells and not the characteristic plasma cells described in previous reports. In such cases, immunohistochemical staining and flow cytometry have an important role in establishing the correct diagnosis. All such patients should undergo a complete workup for multiple myeloma. This guides therapy since localized disease has better prognosis due to its good response to radiation. This case highlights the importance of considering other causes of pancreatic head mass than an adenocarcinoma in a patient with obstructive jaundice.
Acknowledgements
The authors want to thank Dr. Jagbir Sandhu for providing the histology slides.
Disclosure: The authors declare no conflict of interest.
References
- Kyle RA, Rajkumar SV. Multiple myeloma. Blood 2008;111:2962-72. [PubMed]
- Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 2003;78:21-33. [PubMed]
- Bladé J, Kyle RA. Multiple myeloma in young patients: clinical presentation and treatment approach. Leuk Lymphoma 1998;30:493-501. [PubMed]
- Hirata S, Yamaguchi K, Bandai S, et al. Secondary extramedullary plasmacytoma involving the pancreas. J Hepatobiliary Pancreat Surg 2002;9:111-5. [PubMed]
- Tsang RW, Gospodarowicz MK, Pintilie M, et al. Solitary plasmacytoma treated with radiotherapy: impact of tumor size on outcome. Int J Radiat Oncol Biol Phys 2001;50:113-20. [PubMed]
- Varettoni M, Corso A, Pica G, et al. Incidence, presenting features and outcome of extramedullary disease in multiple myeloma: a longitudinal study on 1003 consecutive patients. Ann Oncol 2010;21:325-30. [PubMed]
- Bladé J, Fernández de Larrea C, Rosiñol L, et al. Soft-tissue plasmacytomas in multiple myeloma: incidence, mechanisms of extramedullary spread, and treatment approach. J Clin Oncol 2011;29:3805-12. [PubMed]
- Bachar G, Goldstein D, Brown D, et al. Solitary extramedullary plasmacytoma of the head and neck--long-term outcome analysis of 68 cases. Head Neck 2008;30:1012-9. [PubMed]
- Nolan KD, Mone MC, Nelson EW. Plasma cell neoplasms. Review of disease progression and report of a new variant. Surg Oncol 2005;14:85-90. [PubMed]
- Fischer A, Suhrland MJ, Vogl SE. Myeloma of the head of the pancreas. A case report. Cancer 1991;67:681-3. [PubMed]
- Mitchell DG, Hill MC. Obstructive jaundice due to multiple myeloma of the pancreatic head: CT evaluation. J Comput Assist Tomogr 1985;9:1118-9. [PubMed]
- Kazama T, Ng CS, Giralt SA. Multiphasic CT and MRI appearances of extramedullary multiple myeloma involving the stomach, pancreas, and bladder. Clin Imaging 2005;29:263-5. [PubMed]
- Balliu E, Casas JD, Barluenga E, et al. Multifocal involvement of the pancreas in multiple myeloma: sonographic, CT, and MR imaging findings. AJR Am J Roentgenol 2003;180:545-6. [PubMed]
- Wilson TE, Korobkin M, Francis IR. Pancreatic plasmacytoma: CT findings. AJR Am J Roentgenol 1989;152:1227-8. [PubMed]
- Miljkovic' M, Senadhi V.. Use of endoscopic ultrasound in diagnosing plasmacytoma of the pancreas. JOP 2012;13:26-9. [PubMed]
- Yoshinaga S, Suzuki H, Oda I, et al. Role of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) for diagnosis of solid pancreatic masses. Dig Endosc 2011;23 Suppl 1:29-33. [PubMed]
- Lopes da Silva R.. Pancreatic involvement by plasma cell neoplasms. J Gastrointest Cancer 2012;43:157-67. [PubMed]
- Bredella MA, Steinbach L, Caputo G, et al. Value of FDG PET in the assessment of patients with multiple myeloma. AJR Am J Roentgenol 2005;184:1199-204. [PubMed]
- Soutar R, Lucraft H, Jackson G, et al. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Br J Haematol 2004;124:717-26. [PubMed]
- Wiazzane N, Chargari C, Plancher C, et al. Helical tomotherapy and systemic targeted therapies in solitary plasmacytoma: Pilot study. World J Radiol 2013;5:248-52. [PubMed]
- Available online: http://www.nccn.org/professionals/physician_gls/pdf/myeloma.pdf