Lung adenocarcinoma with solitary gastric metastasis: a case report with literature review
Introduction
Gastrointestinal metastasis from lung cancer is considered a late stage of the disease with reported incidence of 4-12% (1). Of the gastrointestinal tract, small bowel is the most common site of involvement. Gastric metastasis from lung cancer is detected in 0.2-1.7% cases usually during autopsy (2). Gastric metastatic involvement is most commonly occurring with breast cancer, melanoma, and lung cancer. Most patients are asymptomatic. Gastric metastasis from lung cancer suggests advanced disease and mark poor prognosis. Here in we report a female patient with recently diagnosed lung adenocarcinoma presenting with gastrointestinal bleeding and was found to have gastric metastatic ulcer.
Case
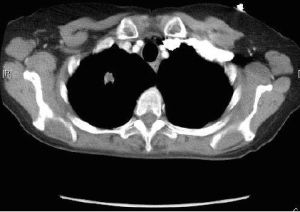
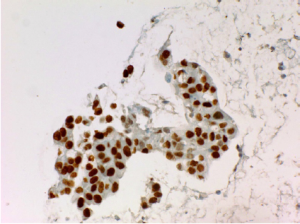
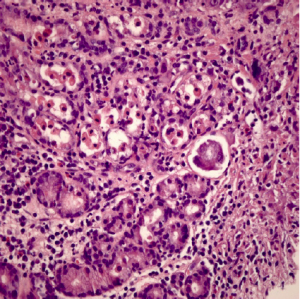
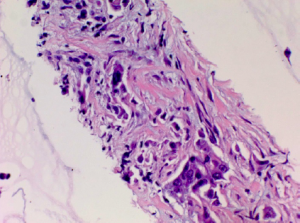
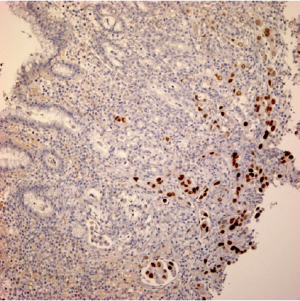
A 60-year-old female presented to the emergency department (ED) with complains of abdominal pain and shortness of breath. Her past medical history was significant for extensive smoking for 36 years, cervical cancer status post hysterectomy with bilateral salpingo-oophrectomy and chemo-radiation 25 years ago, and hypertension. Her medications were Spiriva 18 mcg one inhalation daily, Symbicort, Proventil HFA inhaler two puffs daily, Lisinopril 40 mg once a day. During evaluation in ED, she underwent Chest radiograph which showed right upper lobe speculated mass. She had undergone computed tomography (CT) chest/abdomen/pelvis which showed 1.4 cm speculated mass in right upper lobe, evidence of right suprahilar and azygos adenopathy (Figure 1). She was discharged home with appointments for positron emission tomography (PET) CT and pulmonologist for further diagnostic work up. PET CT scan showed increased radiotracer activity in the right apical nodule which measures 1.4×1.3 cm2, right hilum, pre tracheal lymph node. Patient underwent endobronchial ultrasound (EBUS) with right pre tracheal lymph node biopsy. Biopsy results were positive for adenocarcinoma (Figure 2) and immunohistochemical stains were positive for tissue thyroid factor 1 (TTF-1) (Figure 3) and Napsin A. She was diagnosed with stage IIIA non-small cell lung carcinoma. She underwent port placement and was discharged home with appointments for oncologist and radiation oncologist for further chemotherapy and radiation treatment. She had received few doses of radiation treatment and one month later, she presented to ED again with complain of nausea and hematemesis. She also mentions of syncopal episode at home. In ED, NG tube was placed with return of dark blood. Her Physical exam was significant for pulse 101, blood pressure 94/61 and Conjunctival pallor. Her abdominal exam was not significant for tenderness, guarding or rigidity. Initial laboratory findings revealed blood urea nitrogen 19 mg/dL, creatinine 0.84 mg/dL, INR 1.1, albumin 2.9 g/dL, lactate 0.6 mmol/L, hemoglobin 8.1 g/dL (12.3 three days ago), platelets 304,000 K/uL. Patient was placed on protonix drip and underwent emergent upper endoscopy. Upper endoscopy showed 4 cm wide and 1-2 mm deep ulcer on the lesser curvature with visible vessel which was injected with epinephrine and was cauterized (Figure 4). Biopsies were taken from the ulcer bed and area around the ulcer. Biopsy results were positive for malignant cells histologically and immunohistochemically consistent with metastasis from the lung being primary site of malignancy (Figures 5,6). Patient was transfused with two units of packed red blood cells and observed clinically over next few days. She was discharged home with appointments for oncology for further chemotherapy.
Discussion
Lung carcinoma is the leading cause of death and 40-50% of cases have distant metastasis at the time of diagnosis (3). Gastrointestinal metastasis from primary lung cancer is rare with reported prevalence of 4.7-14% (4). The most common gastrointestinal site of lung cancer metastasis is small bowel. Gastric involvement from lung carcinoma is extremely rare with detection rate of 0.2-1.7% during autopsy (2). Secondary gastric involvement is more common with melanoma, breast cancer, and lung cancer with breast cancer being the most common cause (5). Of the reported lung cancer metastasize to gastrium, large cell carcinoma (3.7%) is the most common followed by adenocarcinoma (2.4%), small cell carcinoma (1.7%), and squamous cell carcinoma (0.7%) (6).
Most patients with gastric metastasis are asymptomatic. Patients tend to have symptoms once gastric mucosa with deeper layer is involved or tumor occupies lumen. The common symptoms of metastasis are bleeding, abdominal pain, obstruction. GI metastasis of lung cancer can cause serious complications, such as perforation, intussusception, and peritonitis (7). The symptoms of nausea and vomiting are unlikely to be investigated with evaluation of gastrointestinal tract because of their consideration as chemotherapy side effect (4).
The mechanism of gastric metastasis could be direct involvement from adjacent organ, or disseminated involvement or hematogenous spread (8). Even-though the stomach receives plenty of blood supply, the reason for rarity of metastasis to stomach from lung cancer is not well understood. However, it is suspected that certain cytokines may affect the organ specificity in hematogenous metastasis (8). Hematogenous metastatic tumor cells to the stomach are situated in the submucosal layer and develop into submucosal tumors.
CT scan imaging in gastrointestinal metastasis of lung cancer manifested itself as an intraluminal polypoid mass or wall thickening with variable contrast enhancement patterns, predominantly iso-attenuation (9). Endoscopically, gastric metastasis appears as “volcano-like ulcer” described as submucosal tumors and small ulcerations on the top (10). The “bull’s eye sign”, initially reported by Pomerantz and Margolin in 1962, is a well-known radiographic feature of gastric metastasis (11). Due to few cases and lack of enough clinical evidence, role of positron emission tomography with fluoro-deoxy-d-glucose (PET-FDG) scan is controversial regarding diagnosis of gastrointestinal metastasis (4). Though clinical usefulness of PET-FDG is increasing for pre-operative staging of esophageal cancer.
The majority of gastric metastasis detected so far has been seen in gastric fundus or cardia. The usual location of primary lung tumor was in upper lobe in most reported cases (2). According to Wu et al., solitary gastric metastasis lesions were reported in 94.4% cases and multiple lesions were reported in 5.6% cases (12). The literature review has revealed few cases of lung adenocarcinoma with gastric metastasis which is summarized in Table 1 including our case (12-17).
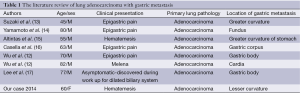
Full table
Lung cancer cases with development of gastrointestinal symptoms after chemotherapy should be carefully evaluated because of two reasons. First reason is nausea and vomiting related to chemotherapy could confound the underlying involvement of gastric region with malignancy in those patients. Another possibility to consider is chemotherapy related ulceration or perforation. With improved chemotherapy for lung cancer, and increased life expectancy, increased number of cases with gastric metastasis may be discovered. Attention needs to be paid to gastrointestinal symptoms and signs in patients with lung cancer.
Conclusions
The prevalence of gastric metastasis from lung cancer is low. Due to asymptomatic involvement in most cases, clinicians need to be vigilant when treating patients with lung cancer. Lung cancer patients with symptoms should be further evaluated with endoscopy. The diagnosis of gastric metastasis signifies advanced disease limiting options of treatment for the patients. The further research in timing of diagnostic and therapeutic strategies is needed to improve outcome.
Acknowledgements
Authors acknowledge help of pathologist Dr. Andrea Lightle to provide slides.
Disclosure: The authors declare no conflict of interest.
References
- Stenbygaard LE, Sørensen JB, Larsen H, et al. Metastatic pattern in non-resectable non-small cell lung cancer. Acta Oncol 1999;38:993-8. [PubMed]
- Ozdilekcan C, Songür N, Memiş L, et al. Lung cancer associated with a single simultaneous solitary metastatic lesion in stomach: a case report with the review of literature. Tuberk Toraks 2010;58:78-84. [PubMed]
- Garwood RA, Sawyer MD, Ledesma EJ, et al. A case and review of bowel perforation secondary to metastatic lung cancer. Am Surg 2005;71:110-6. [PubMed]
- Yang CJ, Hwang JJ, Kang WY, et al. Gastro-intestinal metastasis of primary lung carcinoma: clinical presentations and outcome. Lung Cancer 2006;54:319-23. [PubMed]
- Winston CB, Hadar O, Teitcher JB, et al. Metastatic lobular carcinoma of the breast: patterns of spread in the chest, abdomen, and pelvis on CT. AJR Am J Roentgenol 2000;175:795-800. [PubMed]
- Alpar S, Kurt OK, Ucar N, et al. A case of squamous cell lung carcinoma with gastric metastasis. South Med J 2006;99:1313-4. [PubMed]
- Berger A, Cellier C, Daniel C, et al. Small bowel metastases from primary carcinoma of the lung: clinical findings and outcome. Am J Gastroenterol 1999;94:1884-7. [PubMed]
- Maeda J, Miyake M, Tokita K, et al. Small cell lung cancer with extensive cutaneous and gastric metastases. Intern Med 1992;31:1325-8. [PubMed]
- Kim SY, Ha HK, Park SW, et al. Gastrointestinal metastasis from primary lung cancer: CT findings and clinicopathologic features. AJR Am J Roentgenol 2009;193:W197-201. [PubMed]
- Oda Kondo H. Metastatic tumors to the stomach: analysis of 54 patients diagnosed at endoscopy and 347 autopsy cases. Endoscopy 2001;33:507-10. [PubMed]
- Pomerantz H, Margolin HN. Metastases to the gastrointestinal tract from malignant melanoma. Am J Roentgenol Radium Ther Nucl Med 1962;88:712-7. [PubMed]
- Wu MH, Lin MT, Lee PH. Clinicopathological study of gastric metastases. World J Surg 2007;31:132-6. [PubMed]
- Suzaki N, Hiraki A, Ueoka H, et al. Gastric perforation due to metastasis from adenocarcinoma of the lung. Anticancer Res 2002;22:1209-12. [PubMed]
- Yamamoto M, Matsuzaki K, Kusumoto H, et al. Gastric metastasis from lung carcinoma. Case report. Hepatogastroenterology 2002;49:363-5. [PubMed]
- Altintas E, Sezgin O, Uyar B, et al. Acute upper gastrointestinal bleeding due to metastatic lung cancer: an unusual case. Yonsei Med J 2006;47:276-7. [PubMed]
- Casella G, Di Bella C, Cambareri AR, et al. Gastric metastasis by lung small cell carcinoma. World J Gastroenterol 2006;12:4096-7. [PubMed]
- Lee MH, Kim SR, Soh JS, et al. A solitary gastric metastasis from pulmonary adenocarcinoma: a case report. Thorax 2010;65:661-2. [PubMed]