Primary non-metastatic angiosarcoma of the spleen
Introduction
Primary angiosarcoma of the spleen is a diagnosis of exclusion in any case of splenomegaly. Splenic angiosarcoma is an extremely uncommon malignancy (1), with a reported incidence of only 0.14-0.23 cases per million (2). The origin is believed to be from the splenic sinusoidal vascular endothelium, constituting less than 1-2% of all soft tissue sarcomas. The first case was reported in 1879 by Langhans (3), but to date there are less than 200 cases published in literature (4). We wish to report a case of primary non metastatic angiosarcoma of the spleen of a 69-year-old female who presented to our department.
Case report
A 69-year-old post-menopausal lady presented to the hospital with complaints of fatigue and left sided upper abdominal pain over a period of 3 months. Her past history is significant for hypothyroidism on T. Thyroxine. She initially attributed her symptoms of asthenia and fatigue to her hypothyroid status. At the time of presentation to the hospital, her laboratory investigations revealed anemia (Hb, 9.6 gm%) and the other hematological parameters were within normal limits. On physical examination she had a palpable mass in the left upper quadrant extending almost up to the midline and there was no significant peripheral lymphadenopathy.
Ultrasound of the abdomen revealed moderate splenomegaly (17 cm × 15 cm).
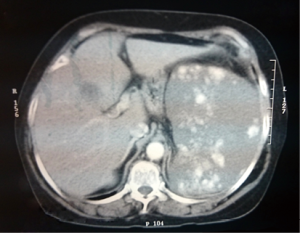
Contrast enhanced computed tomography (CECT) abdomen—spleen shows moderate to gross enlargement with ill defined hypodense lesions in the spleen, multiple central and peripheral irregular intensely enhancing lesions, causing compression of the splenic hilus and indentation of the adjacent left lateral wall of the gastric body (Figure 1). Differential diagnosis were metastasis and angiosarcoma of the spleen.
She was given a shot of pneumococcal vaccine and 1 week later underwent splenectomy through a roof top incision. The enlarged spleen was removed with an intact capsule. Intraoperative and postoperative periods were uneventful.
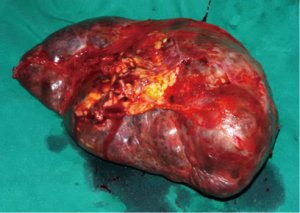
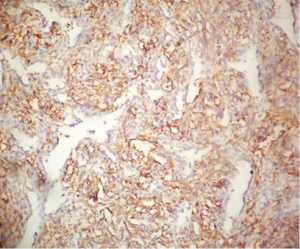
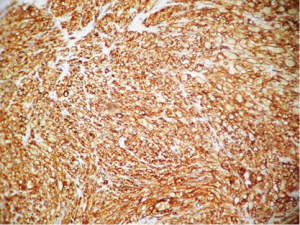
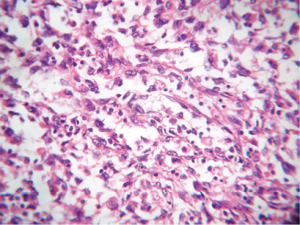
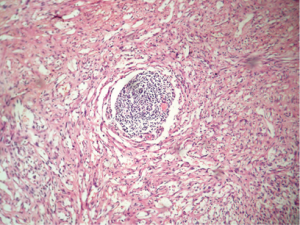
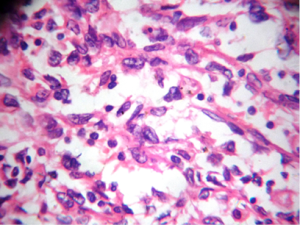
On histopathology, gross appearance revealed splenomegaly measuring 22 cm × 10 cm × 8 cm with intact capsule and bosselated appearance (Figure 2). Serial sections showed diffuse honeycomb appearance with multiple ill-defined fibrous type areas. Microscopic examination revealed the normal architecture of the spleen almost completely replaced by anastomosing vascular channels of varying sizes, lined by atypical proliferating fibroblastic type of cells, with high mitotic activity and areas of necrosis (Figures 3-5). Immunohistochemistry done was positive for CD31 and CD34 (Figures 6,7).
Based upon the above histopathological findings a final diagnosis of angiosarcoma of spleen was made.
A whole body positron emission tomography (PET) CT evaluation was done 3 weeks post operative which ruled out any other site of metastasis.
The patient has been started on adjuvant chemotherapy with doublet of ifosfamide and adriamycin, after a cardiology clearance.
Discussion
Primary angiosarcoma is an extremely rare aggressive malignancy with high metastatic potential. The hypothesized cell of origin is the mesenchymal, elongated endothelial cell lining the splenic sinusoid (1). Published literature, reports a mean age of presentation of 56 years, ranging from 14 months to 89 years, with no sex predilection (2).
Pathogenesis of splenic angiosarcoma is yet to be fully established. Causative agents like thorotrast, vinyl chloride, arsenic etc. that has been attributed to other angiosarcomas, cannot be implicated with the pathogenesis of splenic angiosarcomas (5-9).
The clinical presentation may vary from nonspecific symptoms like fatigue, pain, heaviness to features of hypovolemic shock post splenic rupture. Left sided upper abdominal pain is the most common presenting symptom. Splenomegaly is the most frequent physical examination finding, seen in more than 70% of the patients. The most common laboratory abnormality reported is anemia (10-12).
Splenectomy is the treatment of choice yet rarely curative and because of its very high metastatic potential (13). The majority of metastasis is to the liver, followed by lung, lymph nodes and bones (14,15). The survival benefit with adjuvant chemotherapy or radiotherapy is doubtful, but many case series have treated patients with polychemotherapy schedules containing ifosfamide, adriamycin and platinum compounds (7). There is no phase 2 or 3 data with regards to the management protocol due to its rare incidence.
Prognosis has been dismal with very short term survival ranging from 2 to 14 months, presentation of splenic rupture carrying the worst prognosis (16). Pathologically tumour size and mitotic count are considered as prognostic factors, while grade of the disease has no prognostic value (17).
Conclusions
Primary splenic angiosarcoma is a highly aggressive, extremely rare vascular malignancy, primarily occurring in adults with no sex predilection. The best chance of maximizing survival is to perform a splenectomy prior to splenic rupture or metastatic dissemination. The role of adjuvant chemotherapy or radiotherapy is still controversial. The role of targeted agents in angiosarcomas is yet to be studied.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Neuhauser TS, Derringer GA, Thompson LD, et al. Splenic angiosarcoma: a clinicopathologic and immunophenotypic study of 28 cases. Mod Pathol 2000;13:978-87. [PubMed]
- Falk S, Krishnan J, Meis JM. Primary angiosarcoma of the spleen. A clinicopathologic study of 40 cases. Am J Surg Pathol 1993;17:959-70. [PubMed]
- Langhans T. Pulsating cavernous neoplasm of the spleen with metastatic nodules to the liver. Virchows Arch Pathol Anat 1879;75:273-91.
- Valbuena JR, Levenback C, Mansfield P, et al. Angiosarcoma of the spleen clinically presenting as metastatic ovarian cancer. A case report and review of the literature. Ann Diagn Pathol 2005;9:289-92. [PubMed]
- Abbott RM, Levy AD, Aguilera NS, et al. From the archives of the AFIP: primary vascular neoplasms of the spleen: radiologic-pathologic correlation. Radiographics 2004;24:1137-63. [PubMed]
- Thompson WM, Levy AD, Aguilera NS, et al. Angiosarcoma of the spleen: imaging characteristics in 12 patients. Radiology 2005;235:106-15. [PubMed]
- Hai SA, Genato R, Gressel I, et al. Primary splenic angiosarcoma: case report and literature review. J Natl Med Assoc 2000;92:143-6. [PubMed]
- McGinley K, Googe P, Hanna W, et al. Primary angiosarcoma of the spleen: a case report and review of the literature. South Med J 1995;88:873-5. [PubMed]
- Smith VC, Eisenberg BL, McDonald EC. Primary splenic angiosarcoma. Case report and literature review. Cancer 1985;55:1625-7. [PubMed]
- Kamocki Z, Steward A, Zaręba KP, et al. Primary splenic angiosarcoma - the same diagnosis yielding two different clinical pictures. Case report. Contemp Oncol (Pozn) 2013;17:218-21. [PubMed]
- Duan YF, Jiang Y, Wu CX, et al. Spontaneous rupture of primary splenic angiosarcoma: a case report and literature review. World J Surg Oncol 2013;11:53. [PubMed]
- Yoshida K, Endo T, Kamata K, et al. A case of angiosarcoma of the spleen with intraperitoneal bleeding. Nihon Shokakibyo Gakkai Zasshi 2014;111:549-56. [PubMed]
- Ferreira BP, Rodler ET, Loggers ET, et al. Systemic therapy in primary angiosarcoma of the spleen. Rare Tumors 2012;4:e55. [PubMed]
- Chen KT, Bolles JC, Gilbert EF. Angiosarcoma of the spleen: a report of two cases and review of the literature. Arch Pathol Lab Med 1979;103:122-4. [PubMed]
- Oztürk E, Mutlu H, Sönmez G, et al. Primary angiosarcoma of the spleen. Turk J Gastroenterol 2007;18:272-5. [PubMed]
- Montemayor P, Caggiano V. Primary hemangiosarcoma of the spleen associated with leukocytosis and abnormal spleen scan. Int Surg 1980;65:369-73. [PubMed]
- Naka N, Ohsawa M, Tomita Y, et al. Prognostic factors in angiosarcoma: a multivariate analysis of 55 cases. J Surg Oncol 1996;61:170-6. [PubMed]