Preliminary results with the use of hyperthermic intraperitoneal intraoperative chemotherapy or systemic chemotherapy in high-risk colorectal cancer patients
Introduction
The most frequent sites of recurrence in colorectal cancer are the liver and the peritoneal surfaces (1-3). During surgical resection cancer emboli from traumatized interstitial tissues, transected lymphatic channels, and venous blood loss may disseminate in the abdominal cavity and may be entrapped in the surrounding peritoneal surfaces. These emboli stimulated by growth factors during wound healing give rise to recurrent tumors. This is more prominent if tumor removal is performed in narrow limits of resection as is the pelvis (4). Total mesorectal excision is effective in reducing the incidence of local-regional recurrences in rectal tumors (5). Extended lymph node resection in colon cancer does not offer any survival benefit but it appears to reduce the incidence of local-regional recurrences (6). Systemic adjuvant chemotherapy improves survival in stage III colon cancer (7). Preoperative irradiation combined with total mesorectal excision decreases the incidence of local-regional recurrence (8,9). Both irradiation and systemic chemotherapy are associated with significant toxicity in contrast to intraperitoneal chemotherapy (7-9). Intraperitoneal chemotherapy has been successfully used in the treatment of peritoneal malignancy for the eradication of microscopic residual tumor (10-12). Similarly, if used as an adjuvant in colorectal cancer, it may eradicate the disseminated cancer emboli from the peritoneal surfaces.
The purpose of the study is to compare the effects of hyperthermic intraoperative intraperitoneal chemotherapy (HIPEC) or systemic adjuvant chemotherapy in high risk patients with locally advanced colorectal cancer after surgical resection of the tumor. The end-point of the study is the analysis of overall survival and recurrences.
Patients and methods
Patients
From 2005 until 2010 patients with locally advanced (T3, T4) colorectal cancer were prospectively included in a non-randomized study to undergo R0 resection and receive either HIPEC (HIPEC group) or systemic adjuvant chemotherapy (Conventional group). Patients over 18 years of age that could undergo major surgery, with satisfactory cardiopulmonary function, without evidence of recent cardiovascular accident during the last 6 months, with normal hepatic-renal function, hematological profile, and satisfactory performance status (Karnofsky performance status >50%) were included in the study. Age below 18 years, presence of metastatic unresectable disease, previous treatment for cancer, presence of a second malignancy at high-risk for recurrence (except for skin basal-cell carcinoma or in-situ cervical carcinoma adequately treated), pregnancy, psychosis, drug or alcohol addiction were exclusion criteria.
The segment of the large bowel proximally to the left colic flexure was considered as the right colon. The segment of the colon proximally to the peritoneal reflexion and distally to the left colic flexure was considered as the left colon, and below the peritoneal reflexion as the rectum. The diagnosis of carcinoma was possible by physical examination, hematological and biochemical examination, tumor markers (CEA, CA 19-9, and CA-125), abdominal and thoracic CT-scan, whole body bone scan, colonoscopy, and biopsy. The protocol was approved by the Ethical Committee of the Hospital and all patients signed an informed consent.
Treatments
After abdominal exploration samples were taken for peritoneal cytology. Total mesorectal excision was performed for middle and low rectal tumors. The preservation of the sphincter was on the judgment of the surgeon. The Coliseum technique (open abdominal method) was used in those patients that received HIPEC. Mitomycin-C (15 mg/m2) was diluted in 2-3 lit of normal saline and administered for 90 min at 42.5-43 °C. The reconstruction of the alimentary tract was made after the completion of HIPEC. Patients in the HIPEC group that were pTNM stage III and IV received additional systemic chemotherapy with 5-FU and isovorine. Stage III patients in the conventional group were treated with additional adjuvant systemic chemotherapy with 5-FU and isovorine. Right colon carcinomas were treated with right or transverse colectomy depending on the anatomic location of the tumor. Left colon carcinomas were treated with left colectomy, and rectal carcinomas were treated with low anterior resection or abdominoperineal resection. In low anterior resections a protective colostomy was always performed. Toxicity was recorded from the time of operation and during follow-up.
Histopathology
All specimens were histopathologically examined and details about T, N, M, degree of differentiation, circumferential margins of resection were recorded.
Follow-up
Follow-up was possible every 4 months during the first year after surgery and every 6 months later by physical examination, hematological-biochemical examination, tumor markers (CEA, CA 19-9, CA-125), thoracic and abdominal CT-scan, and whole body bone scan whenever it was indicated. Colonoscopy was performed once a year after the first year of follow-up. Recurrences and the sites of recurrence were recorded.
Statistical analysis
The proportions of patients with a given characteristic were compared by chi-square analysis or by Pearson’s-test. Differences in the means of continuous measurement were tested by Student’s-t-test. The survival curves were obtained using the Kaplan-Meier method and the comparison of curves was calculated using the log-rank test. Logistic regression analysis made possible multiple analysis of recurrence. A two-tailed P value <0.05 was considered statistically significant.
Results
Forty-one patients were included in the HIPEC group and 40 patients in the conventional group. The mean age of the patients in HIPEC and conventional group was 68.1±11.2 [46-84], and 70.7±11 [38-93] years (P>0.05) respectively. The general characteristics of the patients are listed in Table 1. The groups were different for recurrence, presence of distant metastases, and TNM stage (P<0.05), and were comparable for gender, performance status, ASA-class, hospital mortality, tumor depth, nodal infiltration, degree of differentiation, anatomic distribution, morbidity, and median follow-up time (P>0.05). Five additional patients that were initially included in the HIPEC group were excluded from the analysis because they were found to have pT2N0M0 tumors. Four patients in the HIPEC group were found intraoperatively to have liver metastatic disease that was not detected preoperatively but they underwent R0 resection. These patients were included in the analysis. All surgical operations were R0 resections. All samples for peritoneal cytology were negative for malignancy. Two patients in the HIPEC group were recorded with transient neutropenia grade II.
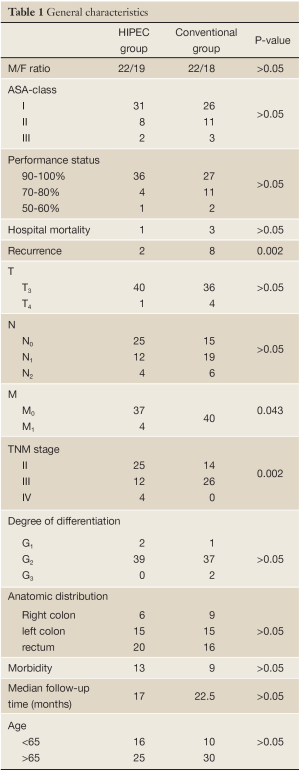
Full table
In both groups median survival was not reached. Although 5-year survival rate for HIPEC group was 100% and for the conventional group 72% the difference was not significant (P=0.0938) (Figure 1). By univariate analysis the nodal status (P=0.003), the stage (P=0.0076), and the degree of differentiation (P<0.0001) were related to survival. By multivariate analysis it was found that the nodal status (HR=6.083, P=0.01, 95% CI, 1.538-24.059) was an independent variable of survival.
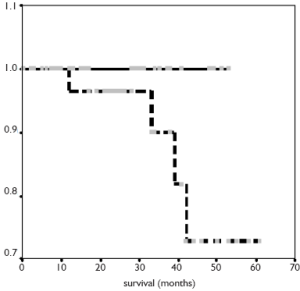 Figure 1. survival of patients in HIPEC group (continuous line), and in group with systemic chemotherapy (dotted line)
Figure 1. survival of patients in HIPEC group (continuous line), and in group with systemic chemotherapy (dotted line)
During follow-up 2 patients in the HIPEC group and 8 patients in the Conventional group were recorded with recurrence (P=0.025). The 2 patients in HIPEC group had undergone surgery for rectal cancer. During initial surgery they were found to have liver metastastatic disease and the disease relapsed again in the liver. Three patients with left-sided colon cancer, 1 patient with right colon cancer, and another one with rectal cancer were recorded with distant metastases in the conventional group. In the same group, 1 patient with rectal cancer, and 2 patients with right colon cancer were recorded with local-regional recurrence. By univariate analysis it was found that the use of systemic adjuvant chemotherapy (P<0.001), the presence of distant metastases (P<0.001), and the stage (P<0.001) were related to recurrence. By multivariate analysis the stage (P=0.002) was identified as the single prognostic variable of recurrence.
Discussion
The preoperative accurate diagnosis of T3 tumors of the colon is very difficult with the current imaging techniques or other diagnostic tools. In contrast, the preoperative definition of T3 or T4 rectal tumors is more accurate by using endoscopic ultrasound or MRI. Therefore, sometimes T2 or even T1 colon tumors may be easily misinterpreted as T3 lesions by preoperative imaging techniques but histopathology provides the definitive data. Therefore, five patients from the HIPEC group were excluded from the study as they were overstaged preoperatively. The groups of the study were comparable. They were different for presence of distant metastases because in the HIPEC group 4 patients were identified with small liver lesions. The metastatic lesions were confirmed histopathologically after adequate resection in all 4 patients. The difference in metastatic disease resulted in the difference in TNM stage between the groups. No difference was recorded for hospital mortality and morbidity as well as in overall survival.
It has long been proved that systemic adjuvant chemotherapy improves survival in stage III colorectal cancer (7) and is the standard of care treatment because it is considered a systemic disease but is not indicated for stage II patients (13). So far intraperitoneal chemotherapy and particularly HIPEC has been effectively used in the treatment of peritoneal carcinomatosis (10-14). It has also been used in patients with locally advanced colorectal carcinomas in whom it appears to improve survival and decrease the incidence of recurrence (15). Local-regional recurrence is usually the result of dissemination of cancer emboli during surgery (4). This may be prevented by using local-regional treatment. In fact the effect of systemic to intraperitoneal chemotherapy has not been compared in regard to local-regional effect.
Although the number of the included patients in both groups is small it appears that overall survival is not influenced by using any of the above treatments. However it seems that the route of administration of chemotherapy plays a significant role in the development of recurrence. It is important to note that no local-regional recurrence was recorded in the HIPEC group in contrast to conventional group in which 3 local-regional relapses were recorded. It has been emphasized that 2 out of 3 of patients with colorectal cancer have developed recurrence at the resection sites (16). Probably HIPEC has no effect in the development of distant metastases but exhibiting a “single pass effect” through the liver in which the drug delivery has been found to be markedly increased may possibly have an advantage in eradicating viable cancer cells that have already disseminated in the liver (17). The local-regional effect of intraperitoneally administered chemotherapy seems to decrease the number of recurrences.
In conclusions, HIPEC as an adjuvant in high risk patients with colorectal carcinomas seems to be effective in reducing the number of recurrences and particularly the local-regional ones. Further studies with larger number of patients are required to document these results.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Minsky BD, Mies C, Rich TA, et al. Potentially curative surgery of colon cancer: patterns of failure and survival. J Clin Oncol 1988;6:106-18.
- Russell AH, Tong D, Dawson LE, et al. Adenocarcinoma of the retroperitoneal ascending and descending colon: sites of initial dissemination and clinical patterns of recurrence following surgery alone. Int J Radiat Oncol Biol Phys 1983;9:361-5.
- Tong D, Russell AH, Dawson LE, et al. Adenocarcinoma of the cecum: natural history and clinical patterns of recurrence following radical surgery. Int J Radiat Oncol Biol Phys 1983;9:357-60.
- Roberts AB, Sporn MB. Principles of molecular cell biology of cancer: Growth factors related to transformation. In: De Vita VT, Hellman S, Rosenberg SA. eds. Cancer Principles and Practice of Oncology. Philadelphia: JB Lippincott, 1989:67-80.
- MacFarlane JK, Ryall RD, Heald RJ. Mesorectal excision for rectal cancer. Lancet 1993;341:457-60.
- Tentes AA, Mirelis C, Karanikiotis C, et al. Radical lymph node resection of the retroperitoneal area for left-sided colon cancer. Langenbecks Arch Surg 2007;392:155-60.
- Laurie JA, Moertel CG, Fleming TR, et al. Surgical adjuvant therapy of large-bowel carcinoma: an evaluation of levamisole and the combination of levamisole and fluorouracil. The North Central Cancer Treatment Group and the Mayo Clinic. J Clin Oncol 1989;7:1447-56.
- Påhlman L, Bohe M, Cedermark B, et al. The Swedish rectal cancer registry. Br J Surg 2007;94:1285-92.
- Improved survival with preoperative radiotherapy in resectable rectal cancer. Swedish Rectal Cancer Trial. N Engl J Med 1997;336:980-7.
- Elias D, Lefevre JH, Chevalier J, et al. Complete cytoreductive surgery plus intraperitoneal chemohyperthermia with oxaliplatin for peritoneal carcinomatosis of colorectal origin. J Clin Oncol 2009;27:681-5.
- Mahteme H, Hansson J, Berglund A, et al. Improved survival in patients with peritoneal metastases from colorectal cancer: a preliminary study. Br J Cancer 2004;90:403-7.
- Verwaal VJ, Bruin S, Boot H, et al. 8-year follow-up of randomized trial: cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy in patients with peritoneal carcinomatosis of colorectal cancer. Ann Surg Oncol 2008;15:2426-32.
- Benson AB 3rd, Schrag D, Somerfield MR, et al. American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol 2004;22:3408-19.
- Sugarbaker PH, Jablonski KA. Prognostic features of 51 colorectal and 130 appendiceal cancer patients with peritoneal carcinomatosis treated by cytoreductive surgery and intraperitoneal chemotherapy. Ann Surg 1995;221:124-32.
- Tentes AA, Spiliotis ID, Korakianitis OS, et al. Adjuvant perioperative intraperitoneal chemotherapy in locally advanced colorectal carcinoma: preliminary results. ISRN Surg 2011;2011:529876.
- Cass AW, Million RR, Pfaff WW. Patterns of recurrence following surgery alone for adenocarcinoma of the colon and rectum. Cancer 1976;37:2861-5.
- Sugarbaker PH, Graves T, DeBruijn EA, et al. Early postoperative intraperitoneal chemotherapy as an adjuvant therapy to surgery for peritoneal carcinomatosis from gastrointestinal cancer: pharmacological studies. Cancer Res 1990;50:5790-4.


