Giant intramural lipoma causing colonic intussusception with multiple jejunal intussusceptions - a case report
Introduction
Intussusception (L. “intus”- within and “suscipere”- to receive) has been a recognized entity since the late 16th century when it was described by Barbette of Amsterdam and subsequently in more vivid detail by John Hunter in 1789 (1). Despite being one of the most common causes of acute abdomen in children, its occurrence in adults is intriguingly uncommon with this group accounting for only 5% of all intussusceptions (2). Colonic lipomata, though common, rarely form the pathological lead point for intussusceptions. The following report describes a left colonic intussusception around a giant intramural lipoma.
Case report
A 28 year old male presented to the emergency with recurrent episodes of colicky abdominal pain in the left lower abdomen for the past 15 days. He then noticed a lump in the loin a week later which remained constant in size till presentation at our hospital. He also complained of multiple episodes of non-bilious vomiting and a change in character of the pain to a constant dull ache in the same region. There was a history of malaena but no haematochezia was reported. The patient had become obstipated over the past few days. There was no history of fever. No other significant medical history was obtained. The patient appeared dehydrated but was hemodynamically stable. Per abdomen examination revealed a firm, intra-abdominal, non-tender, approximately 10 cm × 5 cm sausage shaped lump occupying the left iliac fossa. It was not mobile and there was no associated organomegaly. There was no clinical evidence of free fluid in the abdomen.
Supine and erect radiographs of the abdomen were obtained in the emergency and showed a few air-fluid levels without any evidence of pneumoperitoneum. Ultrasonography revealed evidence of intussuseption of bowel loops in the central abdomen without any free fluid. Biochemistry panel was within normal limits.
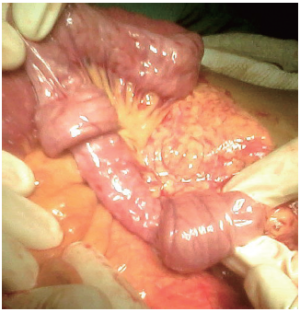
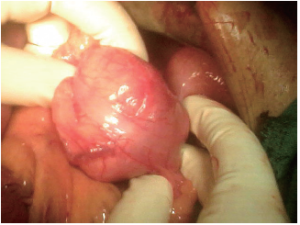
The patient was taken up for laparotomy in view of the clinical picture of bowel obstruction. The possibility of gangrenous intussuscepted bowel was anticipated. On laparotomy, the small bowel loops were grossly normal until the jejunum where multiple intussuscepted bowel segments were seen (Figure 1). Each involved portion showed a variable length of telescoped bowel and two consecutive segments were intussuscepted in both retrograde and antegrade fashion. After gentle reduction, the bowel was found to be healthy and no PLP (pathologic lead point) could be discerned. The caecum, ascending and transverse colon were grossly normal. The descending colon appeared to be the intussusceptum within the intussuscepiens of the sigmoid colon. There was no evidence of strangulation and Cope’s method of reduction yielded a healthy segment of gut with a lead point in the form of an approximately 5 cm × 4 cm intramural lipoma (Figure 2). During dissection, the mucosa was found to be stretched over the lipoma. An inadvertent mucosal breach was repaired primarily and the overlying taenia coli sutured closed with minimal contamination of the peritoneal cavity. The abdomen was closed in layers.
The patient did well post-operatively and moved his bowels by the fourth post-operative day. He was discharged by the sixth post-operative day.
Discussion
The reported incidence of large bowel lipoma, an entity described first by Bauer in 1757 (3), is approximately 0.2-4.4% (4). They are usually asymptomatic. Erkan et al. (5) in a clinicopathologic review of six patients with large bowel lipoma found abdominal pain to be the most frequent symptom with only one requiring emergent intervention in view of acute obstruction. Interestingly, Comfort in 1931 (6) noted that most GI lipomas causing symptoms were at least 4 cm in size although now 2 cm is the accepted dimension (7). Lipomas measuring more than 4 cm are considered “Giant” (8). Other authors have found bleeding per rectum as the most common symptom (54.5%) followed by abdominal pain (42.4%) and alteration of bowel habits (24.2%) (9). Presentation as obstruction, prolapse, perforation or massive haemorrhage is infrequent (10).
Found to be more common in the 5th and 6th decades, there is no consensus as yet regarding the distribution between sexes with some groups claiming a female predominance (11,12). The usual location of the solitary colonic lipoma is the ascending colon (45.5%) and more than 90% occupy the right side, particularly the ileocaecal area. Approximately 6-10% cases have multiple lesions (13). A submucosal location is typical (occasionally extending into the muscularis propria), and up to 10% are subserosal (14).
Adult colonic intussesceptions usually occur around neoplasms of which, 33-75% are malignant such as primary adenocarcinoma, lymphoma and metastatic disease (15). Amongst benign lesions, lipomata, stromal tumors, adenomatous polyps, endometriosis, and previous anastomoses represent common PLPs. Various imaging modalities can aid in the definitive diagnosis of intussuscepted bowel but only histopathology can conclusively prove the etiology. In this case we had to rely on the clinical presentation along with a radiographic picture suggestive of bowel obstruction. The ultrasonographic finding of “bowel within bowel” gave us a working diagnosis and prepared us for the possible findings on laparotomy. A typical concentric hyperechoic double ring coupled with thickening of the intestinal walls is suggestive of colonic intussusception (16). A lipoma appears as an ovoid, well-demarcated filling defect on barium enema with a characteristic “squeeze-sign” as the lesion is deformed by peristalsis. Computerized tomography (CT) can identify colonic lipomas conclusively due the characteristic density of fat (–80 to –120 HU). Gollub outlined the criteria for identifying colonic intussusception as “colon-within-colon or small bowel-within-colon appearance over a length of at least 10 mm on axial CT including mesenteric fat and vessels in the lumen of the intussuscipiens, or an obvious intestinal invagination seen in longitudinal perspective if there was a paucity of mesentery or if the mesentery was edematous and no longer of fat density” (17). Barium studies and CT were not performed in our case due to the emergent nature of the patient’s condition.
Characteristic features of a submucosal lipoma on colonoscopy include the “pillow/cushion sign” (indentation on pressure with closed biopsy forceps and resumption of shape on release), “tenting effect” (tent like appearance on grasping overlying mucosa with forceps) and the “naked fat sign” (protrusion of tissue through the biopsy site) (3). Biopsy is unlikely to provide adequate tissue as the lesion is in fact covered by normal/ulcerated mucosa.
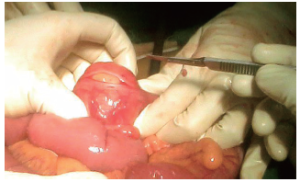
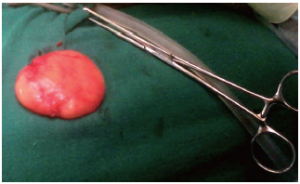
The endoscopic removal of colonic lipoma of even up to 3.8 cm has been performed (18). The risk of haemorrhage or perforation always exists in theory and is increased if the lesion is sessile, intramural or more than 2 cm in size. Jiang et al. (9) suggest surgical removal in the following scenarios - (I) lipoma with a diameter of >4 cm, with a sessile appearance or limited pedicle; (II) unclear preoperative diagnosis; (III) lesions with significant symptoms, especially the appearance of intussusception; (IV) involvement of the muscular layer or serosa; and (V) lesion cannot be resected radically under colonoscopy. In our case, enucleation was attempted and completed due to the ease of dissection and a gross appearance suggestive of a benign pathology (Figure 3). Pathological examination showed a single fibrofatty soft tissue (5.5 cm × 4 cm × 1.5 cm) with a histological appearance of lipoma (Figure 4).
We were hard-pressed to explain the multiple jejunal intussusceptions. It was perhaps due to vigorous retrograde peristalsis in the face of lower intestinal obstruction. Other options for treatment of large-bowel lipomas include hemicolectomy and limited resection by open or laparoscopic techniques with the choice being dictated by pre- or intra-operative findings.
Acknowledgements
Disclosure: It is certified that this manuscript has been read and approved by all the authors. The authors declare that they have no conflict of interest.
References
- Hunter J. On introsusception. Trans Soc Improv Med Surg Knowledge 1793;1:103.
- Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg 1997;173:88-94.
- Ryan J, Martin JE, Pollock DJ. Fatty tumours of the large intestine: a clinicopathological review of 13 cases. Br J Surg 1989;76:793-6.
- Bardají M, Roset F, Camps R, et al. Symptomatic colonic lipoma: differential diagnosis of large bowel tumors. Int J Colorectal Dis 1998;13:1-2.
- Erkan N, Caliskan C, Vardar E, et al. Lipoma of the large intestine: A clinicopathological review of 6 cases. Balkan Med J 2010;27:6-10.
- Comfort MW. Submucous lipomas of the gastrointestinal tract: report of 28 cases. Surg Gynec Obstet 1931;52:101-18.
- Rodriguez DI, Drehner DM, Beck DE, et al. Colonic lipoma as a source of massive hemorrhage. Report of a case. Dis Colon Rectum 1990;33:977-9.
- Bahadursingh AM, Robbins PL, Longo WE. Giant submucosal sigmoid colon lipoma. Am J Surg 2003;186:81-2.
- Jiang L, Jiang LS, Li FY, et al. Giant submucosal lipoma located in the descending colon: a case report and review of the literature. World J Gastroenterol 2007;13:5664-7.
- Vasiliadis K, Katsamakas M, Nikolaidou A, et al. Submucosal lipoma of the ascending colon as a source of massive lower gastro-intestinal bleeding: a case report. Acta Chir Belg 2008;108:356-9.
- Rogy MA, Mirza D, Berlakovich G, et al. Submucous large-bowel lipomas--presentation and management. An 18-year study. Eur J Surg 1991;157:51-5.
- Radhi JM. Lipoma of the colon: self amputation. Am J Gastroenterol 1993;88:1981-2.
- Zhang H, Cong JC, Chen CS, et al. Submucous colon lipoma: a case report and review of the literature. World J Gastroenterol 2005;11:3167-9.
- De Beer RA, Shinya H. Colonic lipomas. An endoscopic analysis. Gastrointest Endosc 1975;22:90-1.
- Lorenzi M, Iroatulam AJ, Vernillo R, et al. Adult colonic intussusception caused by malignant tumor of the transverse colon. Am Surg 1999;65:11-4.
- Alkim C, Saşmaz N, Alkim H, et al. Sonographic findings in intussusception caused by a lipoma in the muscular layer of the colon. J Clin Ultrasound 2001;29:298-301.
- Gollub MJ. Colonic intussusception: clinical and radiographic features. AJR Am J Roentgenol 2011;196:W580-5.
- Kim CY, Bandres D, Tio TL, et al. Endoscopic removal of large colonic lipomas. Gastrointest Endosc 2002;55:929-31.