Cytoreductive surgery using peritonectomy and visceral resections for peritoneal surface malignancy
Introduction
As cancer surgery expanded in the midst of a technological revolution in patient care, this discipline accepted responsibilities not only for the resection of primary tumor but also the surgical management of metastatic disease. Aggressive management strategies to bring about long-term survival to patients with peritoneal surface malignancy have been pioneered by our group (1,2). Successful treatment of abdominal and pelvic malignancies that disseminate to peritoneal surfaces has resulted from extensive experience with appendiceal cancer. Appendiceal cancer became the paradigm for successful treatment of peritoneal metastases (PM) (3,4). This review presents the concepts for and the technique of cytoreduction that prepares the patient for chemotherapy used in the operating room with hyperthermia with acceptable morbidity and mortality.
Principles of management
The successful treatment of peritoneal surface malignancy requires a comprehensive management plan that utilizes cytoreductive surgery (CRS) and perioperative chemotherapy. In addition, proper patient selection is mandatory. Complete resection of all visible malignancy is essential for treatment of peritoneal surface malignancy to result in long-term survival. Up to five peritonectomy procedures may be required (5). The visceral resections and parietal peritonectomy procedures that one must utilize to adequately resect all visible evidence of disease are illustrated below (Table 1). Their utilization depends on the distribution and extent of invasion of the malignancy disseminated within the peritoneal space. Normal peritoneum is not excised, only that which is implanted by cancer.

Full Table
Peritonectomy procedures and visceral resections
In order to manage patients with peritoneal surface malignancy, knowledge regarding the patterns of dissemination of cancer on peritoneal surfaces is necessary. It is imperative that the surgeon develop the technical skills and should be proficient in dissection using electrosurgery.
Rationale for peritonectomy procedures
Peritonectomy procedures are necessary if one is to successfully treat peritoneal surface malignancies with curative intent. Peritonectomy procedures are used in the areas of visible cancer progression in an attempt to leave the patient with only microscopic residual disease. Isolated tumor nodules are removed using electroevaporation; involvement of the visceral peritoneum frequently requires resection of a portion of the stomach, small intestine, or colorectum. Layering of cancer on a peritoneal surface or a portion of the bowel requires peritonectomy or bowel resection for complete removal.
Locations of peritoneal surface malignancy
Peritoneal metastases, especially mucinous carcinomatosis, tend to involve the visceral peritoneum in greatest volume at three anatomic sites (6). These are sites where the bowel is anchored to the retroperitoneum and peristalsis causes less motion of the visceral peritoneal surface. The rectosigmoid colon, as it emerges from the pelvis, is a non-mobile portion of the bowel. Also, it is located in a dependent site and therefore is frequently layered by peritoneal metastases. Usually, a complete pelvic peritonectomy requires stripping of the pelvic sidewalls, the peritoneum overlying the bladder, the cul-de-sac, and resection of the rectosigmoid colon. The ileocecal valve is another area where there is limited mobility. Resection of the terminal ileum and a small portion of the right colon are often necessary. A final site often requiring resection is the antrum of the stomach which is fixed to the retroperitoneum at the pylorus. Tumor coming into the foramen of Winslow accumulates in the subpyloric space and may cause intestinal obstruction as a result of gastric outlet obstruction (7). Large volumes of tumor in the lesser omentum combined with disease in the subpyloric space may cause a confluence of disease that requires a total gastrectomy for complete cytoreduction.
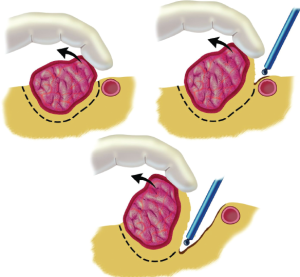
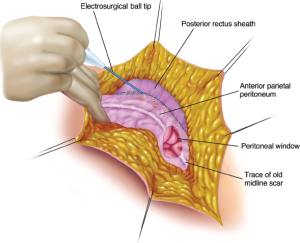
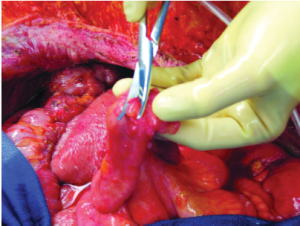
Electroevaporative surgery
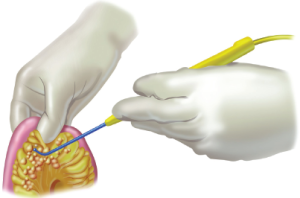
In order to adequately perform peritonectomy, the surgeon must use electrosurgery (8). The electrosurgical handpiece uses a ball tip that allows the tissue surfaces beneath the peritonectomy to be contoured (Valleylab, Boulder, CO). The smooth surface is then able to be resurfaced by peritoneum (Figure 1). Peritonectomies and visceral resections using traditional scissor and knife dissection will unnecessarily disseminate a large number of tumor cells within the abdomen. High voltage electrosurgery leaves a margin of heat necrosis that is devoid of viable malignant cells. Not only does electroevaporation of tumor and normal tissue at the margins of resection minimize the likelihood of persistent disease, but also it minimizes blood loss. In the absence of electrosurgery, profuse bleeding from stripped peritoneal surfaces may occur.
Position and incision
The patient is placed in the supine position with the gluteal fold advanced to the end of the operating table to allow full access to the perineum during the surgical procedure (Figure 2). In the lithotomy position the weight of the legs must be directed to the soles of the feet. Myonecrosis within the gastrocnemius muscle may occur unless the legs are protected properly (9).
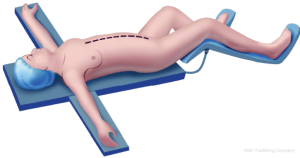
Abdominal skin preparation is from mid-chest to mid-thigh. The external genitalia are prepared in male patients and a vaginal preparation is used in female patients. A Foley catheter is placed and a silastic 18-gauge nasogastric sump tube is placed within the stomach.
Abdominal exposure
The abdominal cavity is opened through a midline incision from xiphoid to pubis. The old abdominal incision is widely excised. The umbilicus is routinely excised but can be reconstructed if the patient desires. The skin edges are secured by heavy sutures to the self-retaining retractor. Traction on the edges of the abdominal incision elevates the structures of the abdominal wall to facilitate their accurate dissection (Figure 3). Strong elevation of abdominal wall helps to avoid damage to bowel loops that are adherent to the anterior abdominal wall (10). Generous abdominal exposure is achieved through the use of a Thompson Self-Retaining Retractor (Thompson Surgical Instruments, Inc., Traverse City, MI).
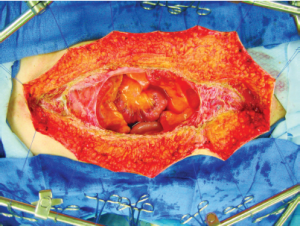
The standard instrument used to dissect the peritoneal surfaces from the normal tissues beneath is a 3 mm ball-tipped electrosurgical handpiece. The ball-tipped instrument is placed at the interface of tumor and normal tissues. The focal point for further dissection is placed on strong traction. The electrosurgical generator is used on pure cut at high voltage. Electroevaporative surgery is used cautiously for tumor removal on tubular structures, especially the ureters, small bowel, and colon. Frequent cooling of the dissection site with room temperature saline will prevent excessive heat accumulation.
Using ball-tipped electrosurgery on pure cut creates a large volume of plume because of the electroevaporation (carbonization) of tissue. To maintain visualization of the operative field and to preserve a smoke-free atmosphere, a smoke filtration unit is used. The vacuum tip is maintained 2-3 inches from the field of dissection whenever electrosurgery is performed (Buffalo Smoke Evacuator, Buffalo, NY).
Xiphoidectomy
If the preoperative radiologic studies suggest the need for right or left subdiaphragmatic peritonectomy, a xiphoidectomy should be performed (11). The midline abdominal incision is extended to approximately four centimeters above the xiphoid-sternal junction. The epigastric fat pad is released from the posterior rectus sheath and a self-retaining retractor is used to widely expose the xiphoid bone and its attachments to the sternum.
Using electrosurgical dissection and progressive advancement of the self-retaining retractor, the xiphoid bone is progressively exposed by releasing it from the anterior and posterior rectus sheath. The dissection is performed with electrocoagulation current on high voltage in order to control the numerous arterial bleeding points that are just lateral to the limits of the xiphoid bone.
After the xiphoid is clearly exposed back to its origins on the sternum, a transverse line of high voltage cutting electrosurgery marks the junction of xiphoid and sternum (Figure 4). The electrosurgical current denatures the protein within the bone at the base of the xiphoid so the bone is fractured precisely with minimal downward pressure at this line.
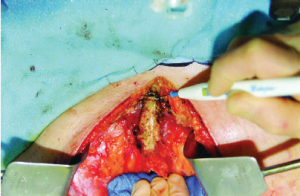
The xiphoid is released from the sternum and its base secured with a Kocher clamp. The broad attachments of the diaphragm muscle to the xiphoid are divided as it is peeled away from the underlying tissues. Care is taken to dissect superior to the diaphragm muscle to avoid entrance into the left pleural space or the pericardial space.
Total anterior parietal peritonectomy
As the peritoneum is dissected away from the posterior rectus sheath a single entry into the peritoneal cavity in the upper portion of the incision (peritoneal window) allows the surgeon to assess the requirement for a complete parietal peritonectomy (Figure 5). If cancer nodules are palpated on the parietal peritoneum, a complete dissection may be indicated to achieve a complete cytoreduction. If the parietal peritoneum is not involved by PM, except for the small defect in the peritoneum required for this peritoneal exploration, the remainder of the peritoneum is maintained intact.
The self-retaining retraction system is steadily advanced along the anterior abdominal wall (Figure 6). This optimizes the broad traction at the point of dissection of the peritoneum from its underlying tissues. The dissecting tool is the ball tip and smoke evacuation is used continuously (12). The superior limit of dissection is achieved with the stripping of the peritoneum from the undersurface of the hemidiaphragm. It is most adherent directly overlying the transversus muscle. In some instances, dissection from inferior to superior aspects of the abdominal wall facilitates clearing in this area. The dissection blends in with the right and left subphrenic peritonectomy superiorly and with the complete pelvic peritonectomy inferiorly. As the dissection proceeds beyond the peritoneum overlying the paracolic sulcus (line of Toldt) the dissection becomes more rapid with the loose connections of the peritoneum at this anatomic site.

Lysis of adhesions
Before proceeding with peritonectomies or visceral resections, all adhesions are separated. As far as is possible these adhesions are resected and submitted as a pathological specimen. After cancer cells have been trapped within the scar tissue, these cancer cells may not be eradicated by the perioperative chemotherapy. The mechanism whereby cancer cells are fixed at sites of prior surgical dissection is referred to as the “Tumor cell entrapment hypothesis”.
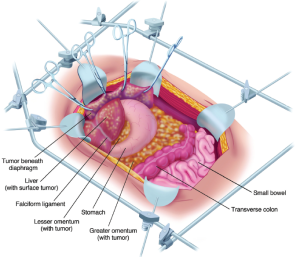
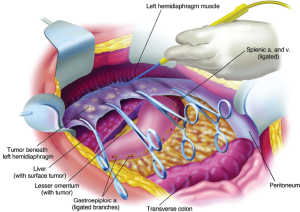
Left subphrenic peritonectomy
The peritonectomy procedures are greatly facilitated by the self-retaining retractor that provides continuous exposure of all quadrants of the abdomen including the pelvis (Figure 7). The epigastric fat and peritoneum at the edge of the abdominal incision are stripped off the posterior rectus sheath. Strong traction is exerted on the tumor specimen throughout the left upper quadrant in order to separate tumor from the diaphragmatic muscle, the left adrenal gland, and the superior half of the perirenal fat. The splenic flexure of the colon is severed from the left abdominal gutter and moved medially by dividing the peritoneum along Toldt’s line. Dissection beneath the hemidiaphragm muscle must be performed with ball-tipped electrosurgery, not by blunt dissection (Figure 8). Numerous blood vessels between the diaphragm muscle and its peritoneal surface must be visualized and individually electrocoagulated before their transection or unnecessary bleeding will occur as the severed blood vessels retract into the muscle of the diaphragm. The plane of dissection is defined using ball-tipped electrosurgery on pure cut, but all blood vessels are electrocoagulated before their division.
Left subphrenic peritonectomy completed
When the left upper quadrant peritonectomy is completed, the stomach may be reflected medially (Figure 9). Numerous branches of the gastroepiploic arteries that have been ligated are evident. The left adrenal gland, pancreas, and left perinephric fat are visualized completely, as is the anterior surface of the transverse mesocolon. The surgeon must avoid the right and left gastric artery and vein to preserve the vascular supply to the stomach.
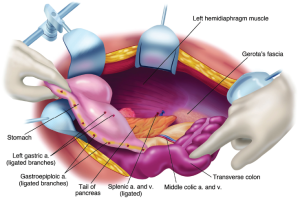
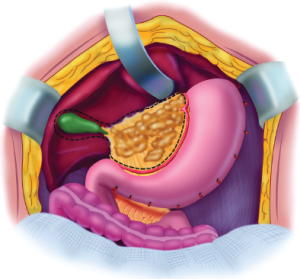
Greater omentectomy and possible splenectomy
To free the mid-abdomen of a large volume of tumor, the greater omentectomy-splenectomy is performed. The greater omentum is elevated and then separated from the transverse colon using electrosurgery. This dissection continues beneath the peritoneum that covers the transverse mesocolon in order to expose the lower border of the pancreas. The branches of the gastroepiploic arcade to the greater curvature of the stomach are ligated in continuity and then divided.
Because the left upper quadrant peritonectomy has been completed, the structures deep beneath the left hemidiaphragm can be elevated. Therefore under direct vision the short gastric vessels are transected. With traction on the spleen, the peritoneum superior to the pancreas may be stripped from the gland bluntly or by using electrosurgery. If the peritoneum covering the pancreas is free of cancer implants it remains intact. The splenic artery and vein at the tail of the pancreas are ligated in continuity and proximally suture ligated. Great care is taken not to traumatize the body or tail of the pancreas.
Right subphrenic peritonectomy
Peritoneum is stripped from beneath the right posterior rectus sheath to begin the peritonectomy in the right upper quadrant of the abdomen. Strong traction on the specimen is used to elevate the hemidiaphragm into the operative field. Again, ball-tipped electrosurgery on pure cut is used to dissect at the interface of tumor and normal tissue. Coagulation current is used to divide the blood vessels between diaphragm and peritoneum as they are encountered and before they bleed.
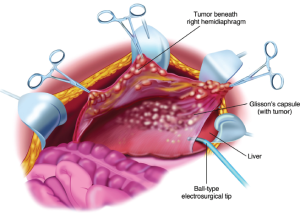
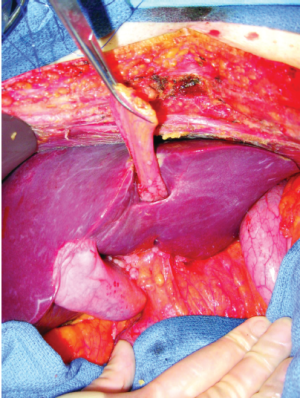
Stripping of tumor from glisson’s capsule
The stripping of tumor from the right hemidiaphragm continues until the bare area of the liver is encountered. At that point, tumor on the superior surface of the liver is electroevaporated until the liver surface is cleared (Figure 10). With ball-tipped electroevaporative dissection, a thick layer of tumor may be bloodlessly lifted off the liver surface by moving beneath Glisson’s capsule (high voltage pure cut electrosurgical dissection). Isolated patches of tumor on the liver surface are electroevaporated with the distal 2 cm of the ball tip bent and stripped of insulation (“hockey-stick” configuration). Ball-tipped electrosurgery is also used to extirpate tumor from attachments of the falciform ligament and round ligament.
Tumor from beneath the right hemidiaphragm, from the right subhepatic space, and from the surface of the liver forms an envelope as it is removed en bloc. The dissection is greatly facilitated if the tumor specimen is maintained intact. The dissection continues laterally on the right to encounter the perirenal fat covering the right kidney. Also, the right adrenal gland is visualized and carefully avoided as tumor is stripped from the right subhepatic space. As the peritoneal reflection at the posterior aspect of the liver is divided, care is taken not to traumatize the vena cava or to disrupt the caudate lobe veins that pass between the vena cava and segment 1 of the liver.
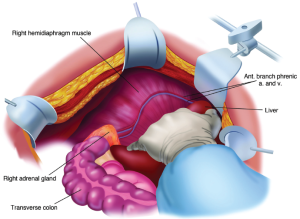
Completed right subphrenic peritonectomy
With strong upward traction on the right costal margin by the self-retaining retractor and medial displacement of the right liver, one can visualize the completed right subphrenic peritonectomy (Figure 11). The anterior branches of the phrenic artery and vein on the hemidiaphragm are seen and have been preserved. The right hepatic vein and the vena cava below have been exposed. The right subhepatic space including the right adrenal gland and perirenal fat covering the right kidney constitutes the base of the dissection.
If the malignancy is invasive, tumor may be densely adherent to the tendinous central portion of the left or right hemidiaphragm. If this occurs, the tissue infiltrated by tumor must be resected. This usually requires an elliptical excision of a portion of the hemidiaphragm on either the right or the left side. The defect in the diaphragm is closed with interrupted sutures. However, the closure occurs after the hyperthermic thoraco-abdominal chemotherapy (HITAC) of both chest and abdomen has been completed (13).
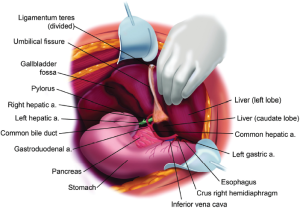
Lesser omentectomy and cholecystectomy with stripping of the hepatoduodenal ligament
The gallbladder is removed in a routine fashion from its fundus toward the cystic artery and cystic duct. These structures are ligated and divided. The hepatoduodenal ligament is characteristically heavily layered with tumor. After dividing the peritoneal reflection onto the liver, the cancerous tissue that coats the porta hepatis is bluntly stripped using a Russian forceps from the base of the gallbladder bed toward the duodenum. The right gastric artery going to the lesser omental arcade is preserved (Figure 12). To continue resection of the lesser omentum, the surgeon separates the gastrohepatic ligament from the fissure that divides liver segments 2 and 3 from segment 1. Ball-tipped electrosurgery is used to electroevaporate tumor from the surface of the caudate process. Care is taken not to traumatize the anterior surface of the caudate process, for this can result in excessive and needless blood loss. The segmental blood supply to the caudate lobe is located on the anterior surface of this segment of the liver, and hemorrhage may occur with only superficial trauma. Also, care must be taken to avoid an accessory left hepatic artery that may arise from the left gastric artery and cross through the hepatogastric fissure. If the artery is embedded in tumor or its preservation occludes clear exposure of the omental bursa, the artery is ligated as it enters the liver parenchyma. It is resected as part of the hepatogastric ligament.
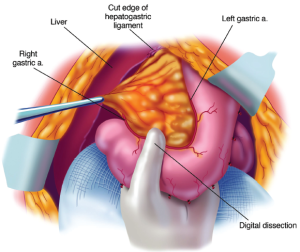
Circumferential resection of the hepatogastric ligament and lesser omental fat by digital dissection
The triangular ligament of the left lobe of the liver was resected in performing the left subphrenic peritonectomy. This completed, the left lateral segment of the liver is retracted left to right to expose the hepatogastric ligament in its entirety. A circumferential electrosurgical release of this ligament (lesser omentum) from the fissure between liver segments 2 and 3, and the left caudate lobe, and from the arcade of right gastric artery to left gastric artery along the lesser curvature of the stomach is required. After electrosurgically dividing the peritoneum on the lesser curvature of the stomach, digital dissection with extreme pressure from the surgeon’s thumb and index finger separates lesser omental fat and tumor from the vascular arcade (Figure 13). As much of the anterior vagus nerve is spared as is possible. The tumor and fatty tissue surrounding the right and left gastric arteries are split away from the vascular arcade. In this manner the specimen is centralized over the major branches of the left gastric artery. With strong traction on the specimen, the lesser omentum is released from the left gastric artery and vein.
Stripping of the floor of the omental bursa
A Dever retractor or the assistant’s fingertips beneath the left caudate lobe are positioned to expose the entire floor of the omental bursa (Figure 14). Further electroevaporation of tumor from the caudate process of the left caudate lobe of the liver may be necessary to achieve this exposure. Ball-tip electrosurgery is used to cautiously divide the peritoneal reflection of liver onto the left side of the subhepatic vena cava. After the peritoneum is divided Russian forceps assist in a blunt stripping of the peritoneum from the superior recess of the omental bursa, from the crus of the right hemidiaphragm, and from beneath the portal vein. Electroevaporation of tumor from the shelf of liver parenchyma beneath the portal vein that connects right and left aspects of the caudate lobe may be required. Care is taken while stripping the floor of the omental bursa to stay superficial to the right phrenic artery.
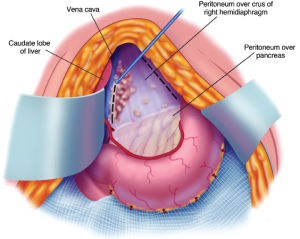
In some patients, a large volume of tumor on the posterior aspect of the hepatoduodenal ligament may be difficult to visualize. A ½ inch Penrose drain placed around the portal triad may allow improved visualization beneath these structures. Using a Russian forceps tearing away the peritoneum beneath the porta hepatis may be necessary under direct visualization. Figure 15 illustrates the complete clearing of the gallbladder, hepatoduodenal ligament, hepatogastric ligament and peritoneal floor of the omental bursa.
Division of the pont hepatique (hepatic bridge) for cytoreduction along the umbilical ligament
The umbilical ligament is a surface structure that defines the separation of the left lateral segment of the liver from liver segment IV. The volume of liver parenchyma that is superficial to the umbilical fissure is extremely variable. Some patients have the umbilical fissure completely open with the umbilical ligament exposed until its entrance into the liver. In other patients a bridge of liver parenchyma covers the umbilical fissure. We refer to this bridge of liver parenchyma as the “Pont hepatique”. The thickness of this bridge of liver parenchyma and the extent to which the umbilical ligament remains visible is extremely variable. Figure 16 shows the pont hepatique covering the umbilical ligament completely in a patient who is having cytoreductive surgery.
The pont hepatique creates a tunnel that surrounds the umbilical ligament. This tunnel is lined by peritoneum and is at risk for seeding by cancer. In order to inspect the peritoneal surfaces within this tunnel, the liver parenchyma above the umbilical ligament must be divided (14).
This is accomplished by ball-tip electrosurgery at high voltage. It can occur in the absence of any bleeding because no major vascular or ductal structures pass through the pont hepatique. After opening the pont hepatique the peritoneal lining of the tunnel it created is carefully inspected. Cancer nodules are electroevaporated from the fissure and the peritoneum peeled away. The presence versus absence of the pont hepatique, the volume of tumor present, and the completeness of cytoreduction at this anatomic site should be recorded in the operative note.
When performing the peritonectomy of the peritoneal lining of the tunnel created by the pont hepatique, there is danger of damage to the left hepatic artery or an early branch of this artery. Special care to visualize and then avoid the left hepatic artery at its entrance into the liver along the umbilical ligament is required in this peritonectomy.
As shown in Figure 17, after division of the pont hepatique, direct vision of tumor nodules within the umbilical fissure is possible. Cytoreduction of these tumor nodules must occur in order to achieve an optimal surgical result. Also, a more complete resection of the umbilical ligament is possible.

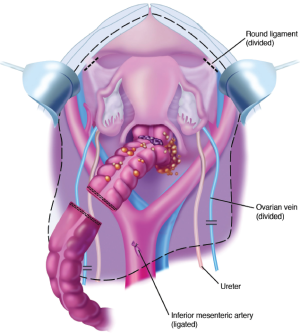
Complete pelvic peritonectomy
The tumor-bearing peritoneum is stripped from the posterior surface of the lower abdominal incision, exposing the rectus muscle. After dissecting generously the peritoneum on the right and left sides of the bladder, the urachus is localized and placed on strong traction using a Babcock clamp. The peritoneum with the underlying fatty tissues are stripped away from the surface of the bladder. Broad traction on the entire anterior parietal peritoneal surface and frequent saline irrigation clears the point for tissue transection that is precisely located between the bladder musculature and its adherent fatty tissue with peritoneum. The inferior limit of dissection is the cervix in the female or the seminal vesicles in the male.
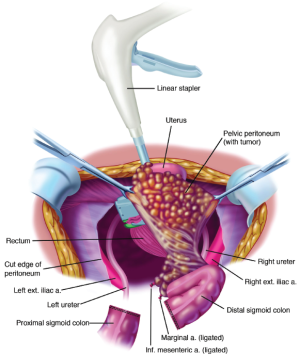
The peritoneal incision around the pelvis is connected to the peritoneal incisions of the right and left paracolic sulci (Figure 18). In the female, the round ligaments are divided as they enter the internal inguinal ring. The right and left ureters are identified and preserved. In women, the right and left ovarian veins are ligated at the level of the lower pole of the kidney and divided. A linear stapler is used to divide the sigmoid colon just above the limits of the pelvic tumor. The vascular supply of the distal portion of the bowel is traced back to its origin on the aorta. The inferior mesenteric artery is ligated, suture ligated and divided. This allows one to pack all the viscera, including the proximal sigmoid colon, in the upper abdomen.
Resection of rectosigmoid colon and cul-de-sac of douglas
Electrosurgery is used to dissect at the limits of the mesorectum. The surgeon works in a centripetal fashion. Extraperitoneal ligation of the uterine arteries is performed just above the ureter and close to the base of the bladder. The bladder is dissected away from the cervix and the vagina is entered. The vaginal cuff anterior and posterior to the cervix is transected using electrosurgery, and the rectovaginal septum is exposed. The perirectal fat is divided beneath the peritoneal reflection so that all tumor that occupies the cul-de-sac is removed intact with the specimen. The rectal musculature is skeletonized using electrosurgery so that a stapler can be used to close off the rectal stump (Figure 19).
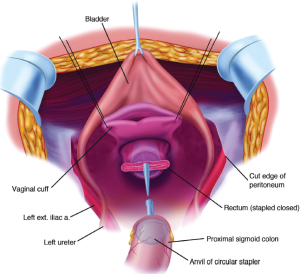
Vaginal closure and low colorectal anastomosis
One of the few suture repairs performed prior to the intraoperative chemotherapy is the closure of the vaginal cuff. If one fails to close the vaginal cuff, chemotherapy solution will leak from the vagina. The circular stapled colorectal anastomosis occurs after the intraoperative chemotherapy has been completed. A circular stapling device is passed into the rectum, and the trochar penetrates the staple line. A purse-string applier is used to secure the staple anvil in the distal descending colon. The body of the circular stapler and anvil are mated and the stapler is activated to complete the low colorectal anastomosis (Figure 20).
Left colon mobilization for a tension-free low colorectal anastomosis
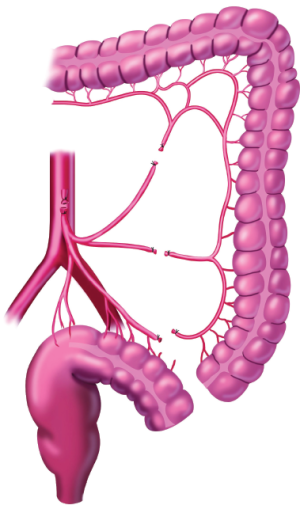
An absolute requirement for a complication-free low colorectal anastomosis is the absence of tension on the staple line. Adequate mobilization of the entire left colon is needed, and several steps may be required to accomplish this. The inferior mesenteric artery is ligated on the aorta, and then its individual branches are resected as they arise from this vascular trunk. The Y-configuration of the left colic and sigmoidal vessels is converted to a V-configuration to keep the intermediate arcade intact (Figure 21). The inferior mesenteric vein is divided as it courses around the duodenum. The mesentery of the transverse colon and splenic flexure are completely elevated from the perirenal fat surrounding the left kidney. Taking care to avoid the left ureter, the surgeon divides the left colon mesentery from all its retroperitoneal attachments. These maneuvers allow the junction of the sigmoid and descending colon to reach to the low rectum or anus for a tension-free anastomosis. Redundant descending colon should fall into the hollow of the sacrum.
To evaluate the stapled colorectal anastomosis, the proximal and distal tissue rings are examined for completeness. Air is insufflated into the rectum with a water-filled pelvis to check for an airtight circle of staples. Two hands should easily pass beneath the sigmoid colon to ensure there is no tension on the stapled anastomosis. A rectal examination is done to check for staple-line bleeding at the anastomosis.
Optimization of cytoreduction of small bowel and its mesentery
The peritonectomy procedures using high-voltage electrosurgery have been applied to the cytoreduction of parietal peritoneal surface malignancy. However, the electrosurgical techniques used in the peritonectomy procedures are not appropriate for the treatment of tumor nodules involving the small bowel. Only a very limited use of electrosurgery on the small bowel itself is possible in order to avoid postoperative fistula. In contrast, small bowel mesentery is an anatomic site for safe use of electroevaporation of cancer nodules (Figure 22).
Five types of small bowel involvement by cancer
CRS with POC has been most commonly used for the management of mucinous appendiceal neoplasms but they have been successfully applied to other tumors, especially colon cancer and diffuse malignant peritoneal mesothelioma. The histological features and the depth of invasion of these different tumors into the bowel wall are not uniform. Based on the extent of the invasion, the size of the tumor nodule and its anatomic location on the bowel wall, small bowel involvement is classified into five types (15):
- Type 1. Non-invasive nodules;
- Type 2. Small invasive nodules on the anti-mesenteric portion of the small bowel;
- Type 3. Moderate size invasive nodules on the anti-mesenteric portion of the small bowel;
- Type 4. All sizes of invasive nodules at junction of small bowel and its mesentery;
- Type 5. Large invasive nodules.
Techniques used in cytoreduction of the small bowel
Type 1. Non-invasive nodules
This type of small bowel involvement involves minute nodules of aggressive histology that because of their small size have not invaded past the peritoneum. It would also include large non-invasive nodules of diffuse peritoneal adenomucinosis or nuclear grade I peritoneal mesothelioma (16,17). The curved Mayo scissors are used to trim these non-invasive nodules from the surface of the small bowel; this results in a localized removal of peritoneum. Larger nodules are frequently scissor-dissected in a piecemeal fashion to avoid damage to the deeper layers of the bowel wall. Considerable skill acquired over time may be needed to avoid damage to the muscularis propria of the bowel (Figure 23). There is usually no need for seromuscular repair.
Type 2. Small invasive nodules on the anti-mesenteric portion of the small bowel
These invasive nodules do not separate from the muscular layer of the small bowel and a partial thickness resection is required. The seromuscular layer is resected leaving mucosa and submucosa intact. This resection is usually performed with a curved Mayo scissor but occasionally it may be performed by pure cut electrosurgery with frequent irrigation to cool the resection site. Scissor or knife dissection is preferred. The seromuscular layer is repaired by suture plication after the intraoperative chemotherapy is completed (Figure 24).

Type 3. Moderate size invasive nodules on the anti-mesenteric portion of the small bowel
In contrast to small invasive nodules in this location, larger nodules require a full thickness elliptical resection of the anti-mesenteric portion of the bowel wall. The closure is performed in two layers and at two different times. The first layer is a full thickness closure using absorbable suture. One suture starts at each corner of the defect and the sutures are then tied at the mid-portion of the resection. Following the POC the defect is closed with a second layer of non-absorbable plication sutures (Figure 25).

Type 4. Small invasive nodules at junction of small bowel and its mesentery
These nodules can sometimes be removed by a localized removal with electrosurgery if sufficiently small and if the vascular supply to the segment of bowel is not compromised. A two-layer repair follows this localized resection. More often, these nodules are removed and the incidence of fistula is reduced by a segmental small bowel resection with end-to-end hand-sewn anastomosis (Figure 26).
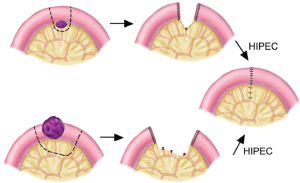
Type 5. Large invasive nodules
These lesions require a segmental small bowel resection with generous proximal and distal margins on the bowel wall and on the mesentery. The segment of small bowel and a portion of its mesentery are resected. The bowel is divided and closed using a linear cutter/stapler. The HIPEC is completed prior to a two-layer hand-sewn anastomosis (Figure 26).
Rationale for perioperative chemotherapy
Current technology for the administration of perioperative chemotherapy demands that it be used as a planned part of the surgical procedure. Several important technological modifications of chemotherapy administration are required. First, an intraperitoneal route for chemotherapy is essential. The intraperitoneal route, when properly utilized, will allow uniform distribution of a high concentration of anticancer therapy at the site of the malignancy. For hyperthermic intraperitoneal chemotherapy this is achieved by the surgeon intraoperatively manipulating the intestinal contents to uniformly distribute the chemotherapy solution. For EPIC given during the early postoperative period, the patient’s position is repeatedly changed to assist gravity in maintaining an optimal chemotherapy distribution.
Secondly, the chemotherapy administration is timed so that all of the peritoneal metastases, except for microscopic residual disease, will have been removed prior to the chemotherapy treatments. This means that the limited penetration of chemotherapy into tissues, which is approximately 1 mm, will be adequate to eradicate all tumor cells. Also, the chemotherapy will be used prior to the construction of any anastomosis. This means that suture line recurrences should also be eliminated. Finally, since all adhesions were resected during cytoreduction, there will be no surfaces in the abdomen or pelvis excluded by scar tissue from contact with chemotherapy solutions.
This comprehensive management plan of CRS and perioperative chemotherapy must be used as early in the natural history of the cancer as is possible. No longer can the clinician wait for the patient with peritoneal metastases to become symptomatic to begin treatments. Even the most aggressive treatment of patients with an invasive malignancy that has a wide distribution of a large mass of cancer will not produce long-term benefits. Peritoneal surface malignancy can be cured, but an optimal result requires that cytoreductive surgery and perioperative chemotherapy to be initiated in a timely fashion.
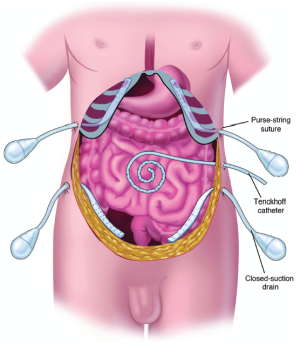
Tubes and drains required for hyperthermic intraperitoneal chemotherapy and early postoperative intraperitoneal chemotherapy
Four closed-suction drains are placed in the dependent portions of the abdomen. This includes one in the right subhepatic space, one in the left subdiaphragmatic space, and two in the pelvis. A Tenckhoff catheter is placed through the abdominal wall and positioned within the abdomen at the site that is thought to be the area of greatest risk for recurrence. All transabdominal drains and tubes are secured at the skin in a watertight fashion with a purse-string suture. Temperature probes are placed at the inflow site (Tenckhoff catheter) and at a remote site (Figure 27). The temperature probes are removed after the intraoperative chemotherapy has been completed but all closed-suction drains are retained. Right angle thoracostomy tubes (Deknatel, Floral Park, NY) are inserted on both the right and left side to prevent abdominal fluid from accumulating in the pleural space as a result of the subphrenic peritonectomy.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Sugarbaker PH. eds. Peritoneal Carcinomatosis: Principles of Management. Boston: Kluwer, 1996.
- Sugarbaker PH. eds. Peritoneal Carcinomatosis: Drugs and Diseases. Boston: Kluwer; 1996.
- Sugarbaker PH, Chang D. Results of treatment of 385 patients with peritoneal surface spread of appendiceal malignancy. Ann Surg Oncol 1999;6:727-31.
- Sugarbaker PH. New standard of care for appendiceal epithelial neoplasms and pseudomyxoma peritonei syndrome? Lancet Oncol 2006;7:69-76.
- Sugarbaker PH. An overview of peritonectomy, visceral resections, and perioperative chemotherapy for peritoneal surface malignancy. In: Sugarbaker PH. eds. Cytoreductive Surgery & Perioperative Chemotherapy for Peritoneal Surface Malignancy. Textbook and Video Atlas. Cine-Med Publishers: Woodbury, CT, 2012.
- Carmignani CP, Sugarbaker TA, Bromley CM, et al. Intraperitoneal cancer dissemination: mechanisms of the patterns of spread. Cancer Metastasis Rev 2003;22:465-72.
- Sugarbaker PH. The subpyloric space: an important surgical and radiologic feature in pseudomyxoma peritonei. Eur J Surg Oncol 2002;28:443-6.
- Sugarbaker PH. Dissection by electrocautery with a ball tip. J Surg Oncol 1994;56:246-8.
- Zappa L, Sugarbaker PH. Compartment syndrome of the leg associated with lithotomy position for cytoreductive surgery. J Surg Oncol 2007;96:619-23.
- Sugarbaker PH. Circumferential cutaneous traction for exposure of the layers of the abdominal wall. J Surg Oncol 2008;98:472-5.
- de Lima Vazquez V, Sugarbaker PH. Xiphoidectomy. Gastric Cancer 2003;6:127-9.
- Vazquez Vde L, Sugarbaker PH. Total anterior parietal peritonectomy. J Surg Oncol 2003;83:261-3.
- Sugarbaker PH, Chang D, Stuart OA. Hyperthermic intraoperative thoracoabdominal chemotherapy. Gastroenterol Res Pract 2012;2012:623417.
- Sugarbaker PH. Pont hepatique (hepatic bridge), an important anatomic structure in cytoreductive surgery. J Surg Oncol 2010;101:251-2.
- Bijelic L, Sugarbaker PH. Cytoreduction of the small bowel surfaces. J Surg Oncol 2008;97:176-9.
- Ronnett BM, Zahn CM, Kurman RJ, et al. Disseminated peritoneal adenomucinosis and peritoneal mucinous carcinomatosis. A clinicopathologic analysis of 109 cases with emphasis on distinguishing pathologic features, site of origin, prognosis, and relationship to “pseudomyxoma peritonei”. Am J Surg Pathol 1995;19:1390-408.
- Cerruto CA, Brun EA, Chang D, et al. Prognostic significance of histomorphologic parameters in diffuse malignant peritoneal mesothelioma. Arch Pathol Lab Med 2006;130:1654-61.


