Radical proximal gastrectomy with modified double tracks anastomosis after preoperative chemotherapy for gastric cancer

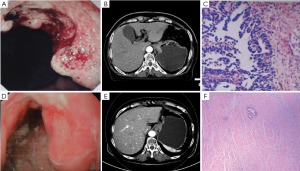
One week later, tests for tumor markers showed: CA50, 9.12 IU/mL; CEA, 2.58 ng/mL; CA19-9, 58.76 IU/mL; and CA72-4, 3.58 U/mL. A second gastroscopy was performed, which showed superficial ulcer at the gastric cardia. The ulcer was fragile and easy to bleed. The diagnosis was gastric cardia cancer, which was pathologically confirmed (Figure 1). CT performed one week after chemotherapy showed post-chemotherapy changes including the thickened gastric walls. The TNM stage was T4N0M0 (Figure 1).
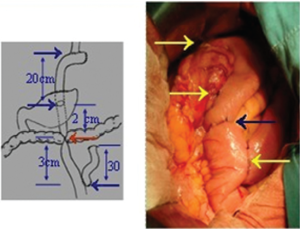
The gastric cancer was down-staged after chemotherapy. The response evaluation was categorized as PR according to RECIST criteria. The surgery was actively prepared. Radical proximal gastrectomy with modified double tracks anastomosis were performed three weeks later (Video 1). An abdominal median incision was routinely made. No ascitic fluid, peritoneal planting, or liver metastasis was found during intra-operative exploration. The tumor (sized 2 cm × 3 cm × 1 cm) was located at the lesser curvature of the gastric cardia, invading the serous membrane. After the removal of greater omentum, gastrocolic ligament, and the anterior lobe of the transverse mesocolon, ligate the left gastroepiploic artery and the short gastric arteries; dissect lymph node stations 4sa and 4sb; ligate the right gastroepiploic vein, and dissect lymph node stations 6 and 4d. The greater curvature of stomach was dissociated. During the treatment of the lesser curvature of stomach, dissect lymph node station 12a; divide the right gastric vessels; and dissect lymph node station 5. The lesser curvature of stomach was dissociated. The stomach was cut at the one third of the line drawn between the larger and lesser curvatures of stomach, and the specimen from the residual tissue was collected. Dissect lymph node stations 8a, 9, 11p, and 11d. Divide the left gastric vein and the left gastric artery, and meanwhile dissect lymph node stations 7, 3, and 1. Dissociate cardia and esophagus, and dissect lymph node station 2. Divide esophagus about 4 cm above the dentate line. Place a T-25 circular stapler into the screw base. Jejunum, mesenteric membrane and its adjacent blood vessels were transected about 30 cm away from the ligament of Treitz. The #29 and #24 stapler were inserted at the distal jejunum about 15-20 cm away from the esophageal-jejunum anastomosis and 5-10 cm away from the antimesenteric border. End-to-side anastomosis was performed between the distal jejunum and esophageal stump across the anterior side of the colon. The jejunal stump was closed using the stump stapler. The seromuscular layer was suture-buried. The lesser curvature of the residual stomach was sutured. Side-to-side anastomosis was performed between the posterior wall of the larger curvature and the distal jejunum using the stapler about 15-20 cm away from the esophageal-jejunum anastomosis. Braun’s anastomosis was performed between the proximal jejunum and the distal jejunum about 5-10 cm away from the gastrointestinal anastomosis. After the jejunal stump was closed using the stump stapler, the seromuscular layer was suture-buried. The intestinal tract 3 cm below the gastrointestinal anastomosis was ligated with a 4-0 silk suture to close the access. All the edges of the anastomosis made by the stapler were continuously sutured. The mesenteric gap was also closed. The surgery was smooth. Mild edema and adhesion of the local tissue were observed. Exudate at the cutting site increased after electric knife or HIFU treatment. The intraoperative blood loss was little. No significantly enlarged lymph node was detected during intra-operative exploration. A limited number of small lymph nodes were dissected. D2 lymphadenectomy was smoothly completed. Satisfactory anastomoses were achieved. The anastomotic tension was low, and the blood supply was good (Figure 2).
Mild hypoproteinemia was detected after surgery and successfully corrected after symptomatic management. No other surgery-related complication occurred. She recovered well and was smoothly discharged. Post-operative pathology: Morphology: a 2 cm × 3 cm × 1 cm superficial ulcer was visible at the lesser curvature of cardia. Its cutting plane was gray and fragile. Histochemistry: CK(+). A small number of degenerative cell variants deep inside deep muscle layer were seen in the tumor bed, and the tumor regression grade (TRG) was TRG 1. Clinically, the lower stump was negative. Detection for positive lymph node showed: CK, negative; station 1, 0/1 (the remaining three were soft tissues); station 2, 0/3; station 6, 0/6; station 11p, 0/2; station 9, 0/1 (the remaining one was soft tissue); station 4sa, 0/5; station 4sb, 0/2; station 3, 0/4 (the remaining one was soft tissue); station 8a, 1; station 11d, 3; station 5, 1; station 19, 1; station 20, 1; station 7, 1; station 4d, 1; station 12a, one soft tissue (Figure 1).
After the treatment, the patient received 6 cycles of adjuvant XELOX, during which mild myelosuppression was observed, which was improved after active interventions. Currently, her quality of life is good, and no relapse or metastasis has been noted.
Acknowledgements
Disclosure: The authors declare no conflict of interest.