Laparoscopy-assisted radical total gastrectomy plus D2 lymph node dissection
Case report

Video description
Patient’s position
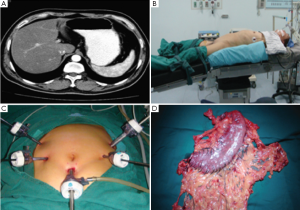
The patient was placed supine and in a split-legged position, with the head slightly higher of 15° (Video 1).
Operator’s positions
The surgeon stood at the left side of the patient, the assistant at the right side of the patient, and the camera holder between her two legs.
Trocar location
Five-hole method was adopted. An annular tube about 10 mm in diameter was placed 1 cm under the umbilicus as the observation hole; a 12-mm cannula is inserted 2 cm to the left anterior axillary line under the costal margin as the main operation hole, and a 5-mm cannula is placed in the left midclavicular line 2 cm above the umbilicus as the traction hole. Two annular tubes about 5 mm in diameter were placed respectively on the right collarbone midline 2 cm above the umbilicus and on the right axillary front 2 cm under the costal margin as the operation holes for the assistant.
Surgical steps
Exploration and separation of gastrocolic ligament
No ascites was found in abdominal cavity and no implantation metastasis nodule was seen in pelvic cavity, omentum and mesentery. No metastatic lesion was found on the liver surface. The tumor was located in the lesser curvature and did not invade the serous membrane. The greater omentum was put on the transverse colon, lifted by the assistant using two non-invasive grasping forceps and simultaneously unwrapped to both sides. The transverse colon was pulled to the opposite direction by the operator using a non-invasive grasping forceps with the left hand to form a triangle traction and keep the tension of the greater omentum. The greater omentum was cut in the avascular zone of superior colon margin near the central part of the transverse colon using an ultrasonic scalpel. After that, the incision was extended to the splenic flexure of colon on the left side and to the hepatic flexure of colon on the right side. The transverse colon margin of the greater omentum was then completely transected.
Separation and dissection of inferior regions of the pylorus
The greater omentum was lifted by the assistant and the transverse mesocolon was pressed by the operator to form certain tension between them and reveal the space formed by the loose connective tissue between the anterior lobe and posterior lobe of the transverse mesocolon. The blunt separation and sharp separation were alternatively used to separate the anterior lobe of the transverse mesocolon using an ultrasonic scalpel along the space from the right margin of the transverse colon to the descendant duodenum on the right side, to the splenic flexure of colon on the left side and to the inferior margin of pancreas on the head side. The middle transverse colon vein was exposed by separating the anterior lobe of the transverse mesocolon. The point of middle colon vein joining the superior mesenteric vein was exposed by separating along the surface of the middle colon vein to the inferior margin of pancreas. The adipose and lymphoid tissues were separated along the anatomic space on the surface of the superior mesenteric vein by the ultrasonic scalpel to the inferior margin of pancreas on the head side. After the retro-pancreatic space was found, the lymphoid tissue was then separated to the left margin of pancreas on the left side and to the point of joining the superior mesenteric vein on the right side. After that, the separation was continued with the ultrasonic scalpel along the anatomic space on the surface of Henle’s axis on the right side to expose the point of the right gastroepiploic vein joining the right/auxiliary right colon vein. The gastric antrum was turned over to the head side and the separated adipose and lymphoid tissue was lifted up by the assistant. And then the separation was continued with the ultrasonic scalpel from the point of the superior pancreas-duodenal vein joining the right gastroepiploic vein to the level of superior margin of pancreatic head along the surface of the right gastroepiploic vein. The completely isolated right gastroepiploic vein was then pulled to the lateral side to be separated from the pancreas by the assistant. The right gastroepiploic vein was transected by the operator on the superior side of the point of super-anterior pancreas-duodenal vein joining the right gastroepiploic vein. The right gastroepiploic vein was then transected after the vascular clamp was used. After that, the gastric antrum was pulled to the head side and the duodenal bulb was pushed to the lateral side by the assistant. The pancreas was lightly pressed by the operator to expose the avascular space between the posterior pancreatic wall and the pancreatic head. And the gastroduodenal artery was exposed by the separation with the ultrasonic scalpel along the space. The root of right gastric artery was exposed after the terminal of gastroduodenal artery was isolated. At this point, the adipose and lymphoid tissues on the surface of the right gastroepiploic artery were pulled by the assistant. The separation was continued along the anatomic space on the arterial surface to the direction of pylorus to isolate the right gastroepiploic artery and cut it at the root after the vascular clamp was used. Here, the inferior pyloric artery from the gastroduodenal artery should also be transected, and damage to the arteries and bleeding should be avoided during the dissection of lymph node station 6. Subsequently, the whole piece of adipose and lymphoid tissue was removed by the ultrasonic scalpel adhering to the duodenal wall from the broken end of the right gastroepiploic arterial root to the isolated duodenal wall to complete the dissection of lymph node station 6. At this point, the dissection of the inferior pyloric lymph nodes was completed.
Dissection of the superior margin of pancreas
The greater omentum was put on the anterior gastric wall in the left and upper stomach and the greater curvature was turned over by the assistant. At the same time, the pancreatic capsule was lifted and tensioned. The transverse mesocolon was pressed under the inferior margin of pancreas by the operator and the pancreatic capsule was then separated carefully by the ultrasonic scalpel adhering to the pancreatic surface to the level of superior margin of pancreas. The gastropancreatic folds were grasped and lifted up by the assistant with the left hand using the grasping forceps and the pancreatic capsule separated to the level of superior margin of pancreas was lifted and tensioned with the right hand. A small gauze was used on the top surface of the pancreas and the pancreas was gently pressed down by the operator to tension the gastropancreatic folds, straighten the left gastric artery and unwrap the superior margin of pancreas. The retro-pancreatic space was entered by opening the gastropancreatic folds with the ultrasonic scalpel along the superior margin of pancreas and usually the splenic artery was firstly exposed. The initiation part of the common hepatic artery could be exposed by separating along the anatomic space on the surface of splenic artery. The adipose and lymphoid tissue on the surface of splenic artery was lifted by the assistant with the right hand using the grasping forceps after the orientation of splenic artery on the superior margin of pancreas was generally understood. The splenic artery was carefully separated along the orientation of splenic artery to the retro-gastric artery branches nearby. After the en bloc removal of the adipose and lymphoid tissues in the proximal splenic artery, the lymph node station 11p was dissected. The dissection of No. 9 lymph node started from the initiation part of splenic artery. The adipose and lymphoid tissue was lifted by the assistant and dissected by the ultrasonic scalpel along the anatomic space on the surface of artery to the direction of the celiac artery. And then the root of the left gastric artery accompanied with the coronary vein was exposed. After that, the adipose and lymphoid tissues around the coronary vein were dissected by the ultrasonic scalpel and the coronary vein was isolated at the level of superior margin of the common hepatic artery followed by the transection. Subsequently, the assistant softly clamped the left gastric artery and pulled it to the head side. The left gastric artery was isolated and transected by the ultrasonic scalpel along its surface to complete the dissection of lymph node stations 7 and 9. The gastropancreatic folds were loosed and the posterior wall of gastric antrum was pulled to the head side by the assistant. And the pancreas was gently pressed by the operator continuously. The separated adipose and lymphoid tissue on the surface of the common hepatic artery was gently lifted by the assistant after the orientation of the common hepatic artery on the superior margin of pancreas was understood. The whole piece of adipose and lymphoid tissue on the superior side of the common hepatic artery was dissected after the separation by the ultrasonic scalpel along the anatomic space on the surface of the common hepatic artery to the direction of duodenum until the point of the common hepatic artery bifurcating gastroduodenal artery and proper hepatic artery to complete the dissection of lymph node station 8a. The posterior wall of the gastric antrum was raised to the head side, and at the same time the duodenal bulb was pushed to the lateral side by the assistant. The pancreas was gently pressed near the bifurcation of common hepatic artery to tension the hepatoduodenal ligament and completely expose the superior region of pylorus from the back. The root of the right gastric artery could be exposed during the process of isolating the proper hepatic artery by the ultrasonic scalpel along the surface of the proper hepatic artery to the direction of porta hepatis. The right gastric artery was gently lifted and isolated carefully by the assistant. And then the vascular clamp was used on the root of the artery for transection. Subsequently, the separation was continued to the right and a “window” was opened on the right side of the anterior lobe of the hepatoduodenal ligament to provide an accurate pointcut for the transection of the hepato gastric ligament. The separated adipose and lymphoid tissue on the surface of the proper hepatic artery was gently lifted by the assistant. The separating was continued by the ultrasonic scalpel to the head side along the anatomic space and the adipose and lymphoid tissues in the anterior reign of the proper hepatic artery and near the root of the right gastric artery were dissected to complete the dissection of lymph node stations 5 and 12a. At this point, the dissection of lymph nodes in the superior margin of the pancreas was completed.
Separation of the hepatogastric ligament
The stomach was turned over to the original place and the transected greater omentum was put in the inferior reign of the colon. The hepatic left lateral lobe was lifted by the assistant and the gastric angle was pressed by the operator to tension the hepato gastric ligament to expose the anterior lobe of the hepatoduodenal ligament. The separation was continued by the operator through the opened “window” of the right anterior lob of the hepatoduodenal ligament to the first porta hepatis. Then the hepato gastric ligament was cut along the inferior margin of the liver to the direction of gastric cardia to complete the dissection of lymph node station 1 and 3.
Separation and dissection of the splenic hilar region
First, it was necessary to change the patient’s and the operator’s stance for the dissection. The patient was in a position of 15-20º head-high and leg-low and 20-30º right inclined. The operator stood between the patient’s legs, and both the assistant and camera holder were on the right side of the patient.
The removed omental tissue was put on the right side in the abdominal cavity, the gastric body was pulled to the right upper side and the left side of the greater omentum was lifted by the assistant. The left transverse colon was pulled to the inferior side and the greater omentum was separated by the ultrasonic scalpel along the superior margin of the transverse colon to the splenic flexure of colon on the left side. The splenogastric ligament was lifted by the assistant and the transverse mesocolon on the splenic flexure was gently pressed to the left and lower side to fully expose the splenogastric ligament and the splenic hilar region. The retro-pancreatic space on the superior margin of the pancreas was entered after the separation of the capsule by the ultrasonic scalpel to firstly expose the splenic vein at the pancreatic tail. The adipose and lymphoid tissues on the surface of the splenic vessels were lifted by the assistant. The separation was continued by the ultrasonic scalpel adhering to the splenic vein to the direction of the splenic hilar and the root of left gastroepiploic vessel could be exposed near the pancreatic tail and the lower pole of spleen. The left gastroepiploic vessel was gently lifted by the assistant and the adipose and lymphoid tissues near the left gastroepiploic vessel were carefully separated by the ultrasonic scalpel. And after the left gastroepiploic vessel was isolated, the vascular clamp was used to block the vessel for the final transection. Then the lymph node station 10 was dissected to the direction of splenic hilar region. The dissection started from the broken end of the left gastroepiploic vessel. The posterior wall of the gastric fundus was pulled and turned over to the right upper side to tension the splenogastric ligament by the assistant. The splenic hilar was then exposed the pancreatic tail and was further pressed by the operator. The adipose and lymphoid tissues on the surface of splenic vascular branch in the splenogastric ligament were gently lifted by the assistant, and the separation was continued carefully by the ultrasonic scalpel adhering to the anatomic space on the surface of the splenic lobar artery. At this point, there were 4-6 short gastric arteries bifurcated from the splenic lobar artery in the splenic hilar region passing through the splenogastric ligament. The short gastric arteries were clamped and pulled to the head side by the assistant. And the adipose and lymphoid tissues were carefully dissected by the ultrasonic scalpel close to the roots of the short gastric arteries. The short gastric arteries were isolated and the vascular clamp was used to block the vessel for the final transection after the passing path was confirmed to the gastric wall. The anterior and posterior regions of splenic lobar artery were isolated continuously and the adipose and lymphoid tissue in the splenic hilar region was fully dissected to complete the dissection of lymph node station 10. It was necessary to notice the variation of the splenic lobar artery branch in the dissection and avoid the bleeding caused by the injury. The transected splenogastric ligament was moved to the anterior wall of the gastric body by the assistant and the gastric fundus was pulled and turned over to the right and upper direction. The trunk of splenic artery in the retro-pancreatic space was exposed after the pancreas was pressed by the operator. The isolated adipose and lymphoid tissue on the surface of the splenic artery was lifted by the assistant. And the adipose and lymphoid tissue around the distal end of the splenic artery was fully dissected along the anatomic space on the surface of the splenic artery from the initial end of the splenic lobe artery to the trunk of splenic artery by the ultrasonic scalpel. At this time, 1-2 posterior gastric arteries bifurcated from the splenic artery were often found. The assistant should clamp the posterior gastric vessels to the upper side for the transection at the roots by the ultrasonic scalpel close to the trunk of splenic artery. The dissection of lymph node station 11d was then completed. Finally the dissection of lymph nodes in the splenic hilar was completed. Subsequently, the gastric fundus wall was pulled to the right and lower sides and the gastrophrenic ligament was separated from the upper pole of the spleen to the esophageal hiatus. The cardiac part of gastric fundus was pulled to the right and upper side by the assistant to expose the left diaphragmatic crus to separate the adipose and lymphoid tissue in the esophageal cardia when the separation continued to the region around the left diaphragmatic crus. It was necessary to notice that there was gastric fundus branch bifurcated from the left inferior diaphragm artery. And it should be isolated at the root to complete the dissection of No. 2 lymph node.
Digestive tract reconstruction
The left and right diaphragmatic crus were isolated and the posterior reign of the esophagus and the right side of the cardia were dissociated. The anterior and posterior branches of vagus nerve were cut and the esophagus was dissociated about 6 cm. The duodenum was cut 3 cm off the pylorus with 60 mm blue nail Endo-Gia stapler closure under the laparoscope and the broken end was closed then. The esophagus was cut 3 cm off the superior margin of the cardia with 60 mm blue nail Endo-Gia stapler closure under the laparoscope and the broken end was closed. The catheter in the OrVilTM stapler resisting the nail seat was slowly delivered to the esophagus stump through the oral cavity with the help of experienced anesthetist. A small incision was made by the ultrasonic scalpel in the corresponding part of the catheter balloon perpendicular to the closed esophageal stump only suitable for the catheter; the catheter was pulled out through the small incision to the abdominal cavity until the white plastic rubber ring was fully exposed. The stitch between the anvil head and catheter was cut to make the anvil head fit the esophagus stump. The catheter was then removed through the main operation hole. A 3 cm longitudinal incision was made under xiphoid in the center of the upper abdomen and the incision protector was implanted. The whole stomach was removed for the pathological examination. The upper jejunum was transected 15 cm below the Treitz ligament through a small incision and the proximal opening hole was closed. The OrVilTM 25 mm stapler was implanted through the distal opening hole of the jejunum. And then the upper abdomen was entered through the small incision. The pneumoperitoneum was reconstructed and the nail seats in the esophageal were anastomosed monitored by the laparoscopy to complete the end-to-side esophageal-jejunum anastomosis. The 60 mm Endo-Gia blue nail was used to close the distal jejunum opening hole. Then the side-to-side esophagus-jejunum anastomosis was performed in the proximal jejunum about 45 cm to the esophagus jejunum. After the abdominal cavity was washed, a drainage tube was placed near the esophagus-jejunum stoma and spleen nest respectively and elicited from the left and right upper abdominal puncture hole to suture the incisions. The post-operative pathology reported pT3N0M0.
Acknowledgements
Disclosure: The authors declare no conflict of interest.


