Epidemiology and burden of colorectal cancer in Asia-Pacific region: what shall we do now?
Introduction
Cancer is an increasingly problem in Asian countries, as similar as western countries because of ageing populations and changes in lifestyle. In this continent which covers approximately 60% of the world’s current human population, only relatively high-income countries including Japan (1), Republic of Korea (2) and Singapore (3), led to the development and implementation of national cancer control plan.
There is an increasing burden of digestive cancer in the world and Asia-pacific region is not an exception. The list of top five most common cancers in Asian countries includes gastric cancer, liver cancer and colorectal cancer (CRC). CRC with high incidence and mortality in Western populations has been extensively studied in these countries. The comparatively low rate is observed in Asian, African, and South America countries; however the past decades have seen a rapid increase of incidence, in Asia-Pacific populations (4). This changing is attributed to environmental factors such as aging and the adoption of the Western lifestyle (5).
In this paper, the epidemiology of CRC and the status of screening strategy for Asia-Pacific region are briefly discussed.
Epidemiology of CRC in Asia-Pacific
CRC is now the third most common malignant disease in both men and women in Asia (5). In the Asia-Pacific region, the incidence varies between regions, with high incidence in Australia, and Eastern Asia, and low incidence in south-central Asia. Data from the Cancer Base of the International Agency for Research on Cancer (IARC) showed that the incidence of CRC in many Asian countries is similar to that in the western ones (6).
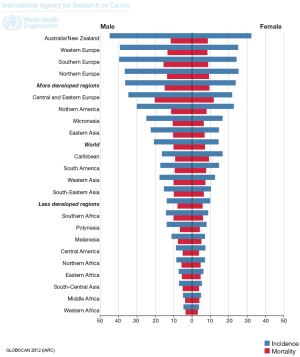
GLOBOCAN estimation project for 2012 indicated that, the age-specific rates (ASR) incidence for Asia was 13.7 and ASR mortality was 7.2 per 100,000. Although the incidence and mortality rate of this cancer are still higher in Western, the ratio of mortality/incidence for Asian regions are higher, which means that the poor survival (Figure 1) (7).
CRC is now the third most common cancer in both sexes in Asia (5) and Eastern Asian countries including China, Japan, South Korea and Singapore showed a two- to four-fold increase in incidence (5). Its incidence is higher among the Chinese (8) and this cancer is one of the three cancers with most rapidly increasing incidence in China, between 1991 and 2005 (9). In Japan and Taiwan an increasing in incidence has also been reported (10,11). In Middle East, the incidence of CRC is increased in Iran, Saudi Arabia and Jordan in recent years (12-15).
The mortality of CRC has been increasing in the last decade in Asian countries, except in Japan and Singapore (5). However, Singapore, Taiwan, and Japan have higher mortality rates for cancer of the colorectal, than the other Asian countries. Studies showed that, the CRC mortality in Hong Kong of China, Japan, South Korea, and Singapore has started to decrease, and the decrease occurred first in the younger age groups (16).
Data from the national mortality routine reporting system in China, indicated that, mortality from CRC has increased through recent decades (17). National death Statistic of Iran reported a slight increasing trend for CRC mortality, and this mortality was higher for older age and male (18,19).
Ethnicity has an important etiological role in CRC in Asia. In Singapore, where different ethnic groups livening in the same environment, the incidence of CRC is lower among the Indian and Malay populations compared to Chinese (8,20) and Chinese people who live in Malaysia, have a significantly higher incidence of CRC than others (20).
Asia-Pacific Cohort Studies Collaboration (involving over half a million subjects from 33 cohort studies in the region of Asia-Pacific) indicated that, smoking, body mass index and lack of physical activity increased risk of CRC in Asia-Pacific region (21).
The incidence, anatomical distribution and mortality of CRC among Asian populations are not different compared with Western countries. There is a trend of proximal migration of colonic polyps and flat or depressed lesions are not uncommon (5). Other risk factors for CRC include family history and metabolic syndrome. First-degree relatives of patients with CRC have a 2-fold increased risk of CRC (22).
Screening
Although, data are lacking in countries such as India and Indonesia, the findings indicate a rapid increasing of CRC burden in Asian countries and there is a need to setup prevention program for this populated region of the world. CRC is an ideal disease for screening. But due to a lack of optimal screening strategy and public acceptance, the universal screening program has not been implemented in most countries. The facilities to access the CRC screening are an important key to reduce the burden of CRC. There are three frequently used screening modalities, namely fecal occult blood tests (FOBT), flexible sigmoidoscopy (FS) and total colonoscopy. Among these three, FOBT is the only method shown in large randomized studies to decrease mortality, using biennial guaiac-based FOBT (23).
A study on cost-effectiveness of FOBT, FS and colonoscopy in Asian countries indicated that FOBT is cost-effective compared to FS or colonoscopy in average-risk individuals aged from 50 to 80 years (24).
The Japan Public Health Center-based Prospective Study group in a cohort study showed a risk reduction in advanced CRC by almost 60% and in mortality by 30% (25). The studies which used screening colonoscopy in Asia showed that the risk of advanced neoplasm tripled after the age of 50 and most guidelines recommend screening to be started at the age of 50 years old (26).
In Asia a minority of population at risk, undergoes screening because of perceived health, access and psychological barriers (27). A survey showed that, men above 50 years of age were particularly unaware of the symptoms of CRC and the benefits of screening (5). A study on 10,078 Chinese revealed that the proportions of perceptual barriers of CRC screening were high among these participants including; financial difficulty, limited service accessibility, screening induced bodily discomfort, etc. (28) and another Chinese study indicated that the uptake of CRC tests was low in the average-risk population (29).
A study in Malaysia showed that the majority of the participants had no knowledge of digital rectal examination, colonoscopy, barium enema and fecal occult blood screening for CRC (30). In Middle East, there is no report for national CRC screening; however, Iranian study suggests it at least for the relatives of CRC patients (31).
The actual uptake and implementation of screening remain low in many Asian countries due to limited resources. National healthcare systems and health insurance are not available to majority of people (5). In most Asian countries, National health-care systems and health insurance cover only a minority of people. So, access to healthcare facilities is limited in many areas and communities of low socioeconomic status (5). Besides, there is little health authority support for CRC screening and very low public awareness of this emerging epidemic in Asia (32). Recommendation for screening by a doctor increases the participation of screening (26). Also study of Asia-Pacific Working Group in CRC revealed that physician recommendation and knowledge of screening tests were significant predictors of CRC test uptake (4). A successful screening program for CRC shall include lack of patient awareness, attitudes and acceptance, physicians’ knowledge, attitudes and recommendations (33). Resource-stratified guidelines from the Asian Oncology Summit 2013 recommend that, people at increased risk of CRC (such as those with personal history or family history of CRC or adenoma) can be screened by colonoscopy. Also genetic test (dependent on the resource available) should be offered to detect increased susceptibility to CRC (34). Besides, the mechanisms involved in CRC initiation and development should be noticed to understanding the burden and prevention strategies for this malignancy. Recent data demonstrated that several genetic and epigenetic changes are important in determining patient prognosis and survival and some of these mechanisms are related to patients’ response to drugs, such as aspirin, which could be used for both prevention and treatment in specific settings (35).
Conclusions
The burden of CRC is still high in Asia-Pacific region and prevention would be one of the best methods to control the disease. It is estimated that over the next two decades the number of CRC cases will increase from 1.2 to 2.2 million worldwide, most of the increase (62%) will be in the developing countries (36) which is the results of westernized life style.
Surveillance system in countries with high burden needed to provide facilities for CRC screening (at least for population at high risks). A problem is that in countries with low facilities, there is also low coverage of cancer registry and the statistics are incomplete or underestimated. Furthermore it is necessary to establish national registry system for countries with low income or help them to estimate truly the burden and epidemiology of CRC, before adjusting any screening plan. CRC screening could be individualized based on genetic or environmental risk factors (for example, in family members of patients, or in those with environmental risk factors) but first we need reliable sufficient data from those populations with different ethnicities and lifestyles (37,38).
Also public awareness education program shall be considered in national and international plane to increases the self-participation of people. The experiences from countries with good CRC prevention system (e.g., Japan, Korea) will be particularly informative to other Asian countries; however financial limitation and lack of authorities are still the main obstacles in the way of CRC screening in most Asian countries with low income status.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Yamaguchi K. Overview of cancer control programs in Japan. Jpn J Clin Oncol 2002;32:S22-31. [PubMed]
- Yoo KY. Cancer control activities in the Republic of Korea. Jpn J Clin Oncol 2008;38:327-33. [PubMed]
- Hock LC. An overview of the cancer control programme in Singapore. Jpn J Clin Oncol 2002;32:S62-5. [PubMed]
- Koo JH, Leong RW, Ching J, et al. Knowledge of, attitudes toward, and barriers to participation of colorectal cancer screening tests in the Asia-Pacific region: a multicenter study. Gastrointest Endosc 2012;76:126-35. [PubMed]
- Sung JJ, Lau JY, Goh KL, et al. Increasing incidence of colorectal cancer in Asia: implications for screening. Lancet Oncol 2005;6:871-6. [PubMed]
- Ferlay J, Bray F, Pisani P, et al. eds. GLOBOCAN 2002: Cancer incidence, mortality and prevalence worldwide, version 2.0. IARC Cancer Base No.5. Lyon: IARC Press, 2004.
- GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012. Available online: http://globocan.iarc.fr/Default.aspx
- Lee HP, Lee J, Shanmugaratnam K. Trends and ethnic variation in incidence and mortality from cancers of the colon and rectum in Singapore, 1968 to 1982. Ann Acad Med Singapore 1987;16:397-401. [PubMed]
- Lu JB, Sun XB, Dai DX, et al. Epidemiology of gastroenterologic cancer in Henan Province, China. World J Gastroenterol 2003;9:2400-3. [PubMed]
- Yiu HY, Whittemore AS, Shibata A. Increasing colorectal cancer incidence rates in Japan. Int J Cancer 2004;109:777-81. [PubMed]
- Yang L, Parkin DM, Li LD, et al. Estimation and projection of the national profile of cancer mortality in China: 1991-2005. Br J Cancer 2004;90:2157-66. [PubMed]
- Moghimi-Dehkordi B, Safaee A, Zali MR. Prognostic factors in 1,138 Iranian colorectal cancer patients. Int J Colorectal Dis 2008;23:683-8. [PubMed]
- Azadeh S, Moghimi-Dehkordi B, Fatem SR, et al. Colorectal cancer in Iran: an epidemiological study. Asian Pac J Cancer Prev 2008;9:123-6. [PubMed]
- Al-Ahwal MS, Shafik YH, Al-Ahwal HM. First national survival data for colorectal cancer among Saudis between 1994 and 2004: what’s next? BMC Public Health 2013;13:73. [PubMed]
- Ismail SI, Soubani M, Nimri JM, et al. Cancer incidence in Jordan from 1996 to 2009--a comprehensive study. Asian Pac J Cancer Prev 2013;14:3527-34. [PubMed]
- Shin A, Jung KW, Won YJ. Colorectal cancer mortality in Hong Kong of China, Japan, South Korea, and Singapore. World J Gastroenterol 2013;19:979-83. [PubMed]
- Yang L, Parkin DM, Li L, et al. Time trends in cancer mortality in China: 1987-1999. Int J Cancer 2003;106:771-83. [PubMed]
- Pourhoseingholi MA, Faghihzadeh S, Hajizadeh E, et al. Bayesian estimation of colorectal cancer mortality in the presence of misclassification in Iran. Asian Pac J Cancer Prev 2009;10:691-4. [PubMed]
- Pourhoseingholi MA, Faghihzadeh S, Hajizadeh E, et al. Trend Analysis of Gastric Cancer and Colorectal Cancer Mortality in Iran, 1995-2003. Iran J Cancer Prev 2011;1:38-43.
- Lim GC, Yahaya H, Lim TO. eds. The first report of the National Cancer Registry: cancer incidence in Malaysia 2002. Kuala Lumpur: National Cancer Registry of Malaysia, 2002.
- Huxley R; Asia Pacific Cohort Studies Collaboration. The role of lifestyle risk factors on mortality from colorectal cancer in populations of the Asia-Pacific region. Asian Pac J Cancer Prev 2007;8:191-8. [PubMed]
- Johns LE, Houlston RS. A systematic review and meta-analysis of familial colorectal cancer risk. Am J Gastroenterol 2001;96:2992-3003. [PubMed]
- Sung J. Colorectal cancer screening: its time for action in Asia. Cancer Detect Prev 2007;31:1-2. [PubMed]
- Kronborg O, Fenger C, Olsen J, et al. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet 1996;348:1467-71. [PubMed]
- Lee KJ, Inoue M, Otani T, et al. Colorectal cancer screening using fecal occult blood test and subsequent risk of colorectal cancer: a prospective cohort study in Japan. Cancer Detect Prev 2007;31:3-11. [PubMed]
- Ng SC, Wong SH. Colorectal cancer screening in Asia. Br Med Bull 2013;105:29-42. [PubMed]
- Sung JJ, Choi SY, Chan FK, et al. Obstacles to colorectal cancer screening in Chinese: a study based on the health belief model. Am J Gastroenterol 2008;103:974-81. [PubMed]
- Wong MC, Ching JY, Hirai HH, et al. Perceived obstacles of colorectal cancer screening and their associated factors among 10,078 Chinese participants. PLoS One 2013;8:e70209. [PubMed]
- Choi KC, So WK, Chan DN, et al. Gender differences in the use of colorectal cancer tests among older Chinese adults. Eur J Oncol Nurs 2013;17:603-9. [PubMed]
- Al-Naggar RA, Bobryshev YV. Knowledge of colorectal cancer screening among young Malaysians. Asian Pac J Cancer Prev 2013;14:1969-74. [PubMed]
- Pourhoseingholi MA, Zali MR. Colorectal cancer screening: Time for action in Iran. World J Gastrointest Oncol 2012;4:82-3. [PubMed]
- Pourhoseingholi MA. Increased burden of colorectal cancer in Asia. World J Gastrointest Oncol 2012;4:68-70. [PubMed]
- Lieberman DA. Clinical practice. Screening for colorectal cancer. N Engl J Med 2009;361:1179-87. [PubMed]
- Lertkhachonsuk AA, Yip CH, Khuhaprema T, et al. Cancer prevention in Asia: resource-stratified guidelines from the Asian Oncology Summit 2013. Lancet Oncol 2013;14:e497-507. [PubMed]
- Colussi D, Brandi G, Bazzoli F, et al. Molecular pathways involved in colorectal cancer: implications for disease behavior and prevention. Int J Mol Sci 2013;14:16365-85. [PubMed]
- Karsa LV, Lignini TA, Patnick J, et al. The dimensions of the CRC problem. Best Pract Res Clin Gastroenterol 2010;24:381-96. [PubMed]
- Bishehsari F, Mahdavinia M, Vacca M, et al. Epidemiological transition of colorectal cancer in developing countries: environmental factors, molecular pathways, and opportunities for prevention. World J Gastroenterol 2014;20:6055-72. [PubMed]
- Rex DK, Johnson DA, Anderson JC, et al. American College of Gastroenterology guidelines for colorectal cancer screening 2009 Am J Gastroenterol 2009;104:739-50. [PubMed]


