Total gastrectomy with D2 lymphadenectomy
Introduction
Since the surgical procedure of Billroth I was developed in 1881, gastrectomy has been made great improvements. However, in lymph node dissection for gastric cancer, the injuries of proper hepatic artery (PHA) or spleen are occasionally occurred (1-3). This video presents a possibility that applying routine laparoscopic approach in open gastrectomy, also provides a more efficient and secure way for No. 10 and No. 12a lymph node dissection comparing with traditional open surgery (Figure 1).

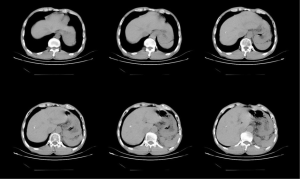
A 63-year-old Chinese male who complained of the light pain in upper left abdomen for 1 month was admitted to local hospital. Gastroscopy revealed a tumor at gastric body and biopsy was taken. Once the pathologic diagnosis of moderately differentiated gastric adenocarcinoma issued, the patient was then referred to our department for further treatment. His post medical history was duodenal ulcer for 10 years, no abdominal operation history or chronic health problems like high blood pressure or diabetes. Physical examination: 168 cm high and 58 kilograms with BMI 20.1 kg/m2, no specific sign was found. Laboratory tests found significantly decreased albumin (34.6 g/L) and slightly decreased erythrocyte (4.12×1012/L). Fecal occult blood testing was negative. Serum tumor markers, including CEA, CA-125 and CA-199, were all in the normal range. Abdominal CT scan (Figure 2) revealed that the lesion, where the gastric wall was thickened, at the lesser curvature of the stomach and near the cardia. Multiple enlarged lymph nodes were found near the lesser curvature region. No distinct liver metastasis or other visceral organ invasion was found.
Exploratory laparotomy was performed on 18th May 2015 after eliminating the contraindication of radical gastrectomy.
Operative techniques
After general anesthesia combined with epidural block performed, the patient with supine posture was explored by a 12 cm median incision in upper abdomen. Following the sequence of from bottom to top and distant to proximal, the primary lesion was finally checked when abdominal and pelvic cavity had been comprehensively examined. At the same time, washing cytology was also performed by saline solution into the abdominal cavity. In this case, the primary tumor was located at the lesser curvature of the stomach and the upper third of gastric body, approximately 2×1.5 cm2 in size, invaded serosa layer. Enlarged lymph nodes could be found near the lesser curvature, but adjacent structures invasion, distant metastasis and washing cytology were negative.
Primary incision lengthened from xiphoid to 1 cm circumumbilically under the navel and covered with incision protector. To obtain a better surgical exposure, two retractors were fastened against bilateral costal margin while three wet gauze pads were placed under the spleen. It efficiently prevents splenic injury during the operation, also provides a favorable way for D2 lymphadenectomy.
Along the descending portion of duodenum, Kocher incision that striped the gap behind duodenum and pancreatic head until to the aortaventralis, was made for freeing duodenum and exploring No. 13 lymph node. The segregation of anterior and posterior lobe of transverse mescaline was begun with the right side of omentum majus between the hepatic flexure and duodenum. For an assistant, held the transverse colon and fanned out the both lobes with a little tension. As an operator, segregation was performed between the lobes by electrotome from right to left until to the inferior border of pancreas. No. 14v lymph node was removed as the suspicion of No. 6 lymph node metastasis. Right gastroepiploic vein was ligatured and severed in front of pancreas head. By routine laparoscopic approach, gastroduodenal artery and right gastroepiploic artery were exposed at upper rim of pancreas for further disposal. Left gastric vein could be easily found during the lymphadenectomy following the sequence of from left to right. Gauze was placed under the right gastric artery after the exposure of PHA and right gastric artery. Lay down the stomach and sectioned the hepatogastric ligament for dissection of No. 12a lymph node. Remove the No. 5 lymph node and cut off the duodenum 3 cm under the pylorus for closing. After showing portal vein and along common hepatic artery, No. 8a lymph node could be safely removed until to left gastric artery. No. 11p lymph node dissection was the last step of lymphadenectomy at right side of abdomen. The stomach and peripheral tissues were wrapped by a gauze pad for preventing inoperative iatrogenic tumor cells dissemination. As shown in the video, splenic hilum was exposed in situ by anterior and posterior pancreatic approach for lymphadenectomy. Moreover, gastroepiploic vessels, the short gastric vessels and No. 4a lymph node were processed at last. Inserting the anvil of stapler in the broken ends of esophagus that severed 5 cm away from the tumor, digestive tract reconstruction was applied by stapler with Roux-en-Y gastrojejunal anastomoses.
Comments
It provides a potential improvement for laparotomy that applying routine laparoscopic approach in open gastrectomy. Anterior and posterior pancreatic approach is also a safe and efficient way for No. 10 lymphadenectomy.
Acknowledgements
This operation was performed with the assistant of Doctor Huang Yingpeng and Pan luofeng, as well as the nurses and anesthetists. The video was produced by Doctor Ma Haiguang.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Park MS, Yu JS, Kim KW, et al. Case report: focal hepatic necrosis as a complication of gastric cancer surgery: imaging features in one patient. Clin Radiol 2002;57:858-60. [PubMed]
- Kitagawa T, Iriyama K. Hepatic infarction as a complication of gastric cancer surgery: report of four cases. Surg Today 1998;28:542-6. [PubMed]
- Ren MY, Huang B, Zhang J, et al. Laparoscopic transhiatal proximal gastrectomy for adenocarcinoma of the esophagogastric junction: report of 98 cases. Zhonghua Wei Chang Wai Ke Za Zhi 2012;15:906-9. [PubMed]
- Chen W, Hu C, Huang Y, et al. Total gastrectomy with D2 lymphadenectomy. Asvide 2015;2:089. Available online: http://www.asvide.com/articles/682


