Metastatic melanoma of ampulla of Vater presenting as obstructive jaundice: case report with literature review
Introduction
The behavior of malignant melanoma is highly unpredictable, with relapses occurring without major warning signs. Melanoma metastasis to gastrointestinal (GI) tract is often asymptomatic and is only discovered post-mortem with the greatest propensity for GI metastasis being to the small bowel (1). When identified ante-mortem, the common presentation is small intestine intussusception or obstruction. However, very few case reports of obstructive jaundice from metastatic malignant melanoma to the ampulla of Vater have been reported. Here in, We present female with history of melanoma presenting with obstructive jaundice and was found to have malignant melanoma at ampulla of Vater by biopsy. Patient was treated with biliary stent placement and currently undergoing chemotherapy under clinical trial and has been doing well for past 11 months since her diagnosis of metastatic ampullary involvement.
Case report
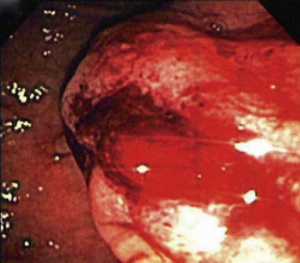
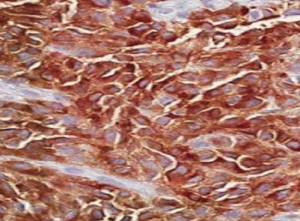
A 58-year-old woman referred to our clinic with complaints of dull, non-radiating right upper quadrant abdominal pain with no major alleviating factors and non-bloody emesis for about 4 weeks duration. She has noticed 3 kilogram of weight loss, light-colored stools and dark urine over the course of 2 weeks. Her medical history was significant for surgical resection of melanoma skin lesions on her low back and left thigh in 1996 and 2003 respectively. On examination patient had icteric sclera. Abdominal examination revealed right upper quadrant and epigastrium tenderness. Blood investigations showed complete blood count (CBC) normal, aspartate aminotransferase (AST) 121 U/L; alanine aminotransferase (ALT) 164 U/L; total bilirubin 4.3 mg/dL and alkaline phosphatase (ALP) 285 IU/L. Abdominal USG on presentation depicted sludge and tiny stones in the gallbladder with abnormally dilated common bile duct and distal common duct obstruction. Endoscopic ultrasound showed prominent ampulla with hypoechoic appearance indicative of an ampullary mass and dilated common bile duct (Figure 1). Subsequent endoscopic retrograde cholangiopancreatography (ERCP) revealed a friable ampullary mass with bleeding (Figure 2) and tight distal common bile duct stricture. Patient underwent sphincterotomy, common bile duct balloon dilation and stent placement and ampullary biopsy. After biopsy results were consistent with malignant melanoma (Figure 3), she was evaluated for a possible Whipple procedure. Preoperative computed tomography (CT) scan showed multiple lung lesions which were suspicious for metastatic disease and therefore a Whipple procedure was not considered. Our patient has entered a clinical trial and is currently undergoing chemotherapy treatment and doing well for past 11 months. She has completed two cycles of chemotherapy with plans to complete total of four cycles followed by repeat imaging of magnetic resonance imaging (MRI) brain and CT chest, abdomen, and pelvis.
Discussion
Melanoma, embryonically derived from the neural crest cells, originates in the pigment producing melanocytes in the basal layer of the epidermis. Malignant melanomas are known for their unpredictable dissemination pattern to virtually any organ, such as the liver, lung and brain. An autopsy study of 216 patients with advanced malignant melanoma revealed GI metastasis is second to the lung in sites of organ metastatic disease (1). The Roswell Park Memorial Institute has sub-classified GI organ involvement in the following distribution: liver, 58.3%; peritoneum, 42.6%; pancreas, 37.5%; small bowel, 35.6%; spleen, 30.6%; colon, 28.2%; stomach, 22.7%; oral cavity and esophagus, 9.3%; and biliary tract, 8.8% (1). While the incidence of metastatic malignant melanoma to the GI tract is well documented, dissemination to the ampulla of Vater resulting in obstructive jaundice is far less common with very few clinical cases reported so far.
Most often, GI metastasis is asymptomatic and is only discovered post-mortem with the greatest propensity for GI metastasis being to the small bowel (2). When identified ante-mortem, the heralding sign is usually small intestine intussusception or obstruction, however GI bleeding is also common. The metastatic lesions are usually multiple, ulcerated or polypoidal, hyper pigmented or amelanotic but rarely solitary (2,3). While the differentiation of a primary GI mucosal melanoma from metastasis to the GI tract can be quite difficult, the presence of junctional melanocytic proliferation supports the diagnosis of a primary mucosal melanoma (2). The primary melanomas of the GI tract have a tendency to be more aggressive, and are associated with a worse prognosis. Malignant melanoma metastatic to the GI tract is usually a late manifestation of the disease with an overall poor prognosis (2).
According to literature search, eight cases reported so far and total nine cases including our case, of which, virtually all the patients presented with painless jaundice (7/9) (Table 1) and had proven primary cutaneous or vaginal melanoma at the time of diagnosis of GI metastasis (7/9) (3-10). In two of the cases despite complete clinical and radiological examinations, the primary lesion was not identified even though the possibility of an undetected or regressed tumor could never be ruled out.

Full table
Diagnostic workup by CT, ultrasonography, barium studies, and endoscopic evaluation should be highly considered at the time of the diagnosis in an effort to identify the primary lesion and rule out other organ metastasis as this could dictate the course of therapy. The sensitivity of detecting metastatic lesion by CT scan is 69-70%, and since negative CT does not rule out diagnosis, further studies should follow negative CT scan results (10). The current gold standard for the diagnosis of melanoma is histopathologic staining such as human melanoma black-45 (HMB-45) and S100 (1).
There are no standard guidelines for optimal treatment due to the rare incidence of melanoma to the ampulla of Vater. Biliary stenting offers temporary symptomatic palliation with a rapid improvement in cholestasis. Surgical treatment such as pancreaticoduodenectomy could be an option for isolated metastatic lesions to the ampulla of Vater in select symptomatic patients with good performance status and no other sites of metastatic disease. However, such procedures are never a curative therapy for metastatic disease.
The overall median survival of metastatic malignant melanoma in the ampulla of Vater ranges from 6-9 months with a 5-year survival rate of less than 10% as demonstrated in several case series (2). So far no randomized clinical trials were able to illustrate mortality benefit with adjuvant therapy. Although the overall prognosis is grim, multidisciplinary approach to treatment of these patients including surgical or endoscopic palliation, immunotherapy, and chemotherapy may enhance short-term survival.
Conclusions
GI melanoma is frequently a result of metastasis and thorough evaluation via physical examination, radiographic studies and endoscopic evaluation is required to identify potential primary site. A high index of suspicion should be given to patients with new onset of vague GI complains because early diagnosis and surgical intervention provides the most effective palliation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Patel JK, Didolkar MS, Pickren JW, et al. Metastatic pattern of malignant melanoma. A study of 216 autopsy cases. Am J Surg 1978;135:807-10. [PubMed]
- Schuchter LM, Green R, Fraker D. Primary and metastatic diseases in malignant melanoma of the gastrointestinal tract. Curr Opin Oncol 2000;12:181-5. [PubMed]
- Fléchon A, Lombard-Bohas C, Saurin JC, et al. Malignant melanoma presenting as an ampullary tumour. Histopathology 2002;41:562-3. [PubMed]
- van Bokhoven MM, Aarntzen EH, Tan AC. Metastatic melanoma of the common bile duct and ampulla of Vater. Gastrointest Endosc 2006;63:873-4. [PubMed]
- Caballero-Mendoza E, Gallo-Reynoso S, Arista-Nasr J, et al. Obstructive jaundice as the first clinical manifestation of a metastatic malignant melanoma in the ampulla of vater. J Clin Gastroenterol 1999;29:188-9. [PubMed]
- Sans M, Llach J, Bordas JM, et al. Metastatic malignant melanoma of the papilla of Vater: an unusual case of obstructive cholestasis treated with biliary prostheses. Endoscopy 1996;28:791-2. [PubMed]
- Uiterwaal MT, Mooi WJ, Van Weyenberg SJ. Metastatic melanoma of the ampulla of Vater. Dig Liver Dis 2011;43:e8. [PubMed]
- Nakayama H, Miyazaki S, Kikuchi H, et al. Malignant vaginal melanoma with metastases to the papilla of Vater in a dialysis patient: a case report. Intern Med 2011;50:345-9. [PubMed]
- Marks JA, Rao AS, Loren D, et al. Malignant melanoma presenting as obstructive jaundice secondary to metastasis to the Ampulla of Vater. JOP 2010;11:173-5. [PubMed]
- Bendic A, Glavina Durdov M, Stipic R, et al. Melanoma in the ampulla of Vater. Hepatobiliary Pancreat Dis Int 2013;12:106-8. [PubMed]