Robotic gastrectomy: where do we stand
Introduction
Minimally invasive surgery has been developed to facilitate patients’ recovery after gastrectomy (1). The first use of laparoscopic surgery for gastric cancer was reported in 1994, since then it has become widely used for the treatment of gastric cancer. Much evidence has accumulated with minimally invasive gastrectomy, which supports the short-term benefits including shorter hospital stays and lower postoperative complication rates for early gastric cancer patients while maintaining comparable oncologic safety (1,2).
However, laparoscopic surgery has many technical limitations such as two-dimensional imaging, restricted range of motion, amplified hand tremors can be problematic when performing complex surgery procedures for gastric cancer (2-4). The robotic surgery system which allows motion scaling, three-dimensional visualization and a high degree of freedom was introduced as a solution to minimize the shortcomings of laparoscopy (2,3). Robotic surgery using the da Vinci surgical system is anticipated to be a powerful tool for performing difficult techniques but, definite superiority to laparoscopic gastrectomy (LG) is yet to be proven. There are many issues concerning robotic gastrectomy (RG) when comparing it to LG, some of these issues are (I) learning curve, (II) lymph node dissection, (III) short-term outcomes, (IV) long-term outcome, and (V) cost. Hence, whether RG has superiority in those issues compared to LG needs to be verified and this what we are going to describe in this review.
Learning curve of RG
Recently, almost all articles reported robotic surgery requires a shorter learning curve than laparoscopic surgery, particularly in cases of radical gastrectomy and lymphadenectomy for gastric cancer, and that is regarded as one of its principal advantages (1,4-11). This is thought to be due to the easier maneuverability and adaptability of the da Vinci system and easy adaptation to RG by laparoscopic surgeons because the operating procedure and scope view of robotic-assisted gastrectomy are similar to those of laparoscopic-assisted gastrectomy (4,9).
The mean number of procedures performed until the operative time stabilized was fewer than laparoscopic procedure. In addition, RG learning curve reaches a plateau much faster and the time required to achieve proficiency for robotic surgery is shorter than that for LG. Therefore, surgeons with sufficient experience in LG are able to rapidly overcome the learning curve for RG (6). A total of 40-60 cases of surgical experience are needed to stabilize the operating procedure and time related to LG (1,4,10), but 11-25 cases are needed for RG (1,10,11).
Shorter learning curve is associated with potential of diffusion and reproducibility of the surgery. Therefore, easy and rapid learning of robotic surgery can help the expansion and standardization of the minimally invasive surgery to gastric cancer treatment (1,9). It would be easier for inexperienced surgeons to adopt minimally invasive surgical techniques and this might also result in experienced surgeons more easily adopting advanced or complicated procedures for gastric cancer treatment (1).
However, most of the results are collected from highly professional laparoscopic gastric surgeons (1,9). To accurately evaluate and compare the learning curves of minimally invasive gastrectomy, a well-designed randomized control study is needed.
Lymph node dissection
Robotic surgery could show superiority in procedures which need more advanced techniques because forceps in robotic surgery can be maneuvered with a higher degree of freedom than in laparoscopic surgery. It can lead to better oncological outcome in the treatment of gastric cancer especially for total gastrectomy which required more advanced skills (5,8). Laparoscopic total gastrectomy, has technical difficulties regarding reconstructive techniques and lymph node dissection around the splenic artery and splenic hilum area particularly (5). For early gastric cancer with lymph node metastasis or advanced gastric cancer, D2 dissection is recommended and when performing D2 dissection, lymph node dissection of the superior border of the pancreas, which is most crucial when treating gastric cancer, dissection must include the tissues behind the pancreas, common hepatic artery, and splenic artery. Because LG requires high level of skills in lymph node dissection at those areas, therefore, robotic advantages are anticipated to allow harvesting more number of lymph nodes (5,6). For example, the EndoWrist® (Intuitive Surgical, Sunnyvale, CA, USA) function of robotic system allows the surgeon to reach deep areas that could not be approached easily and accurately with the straight forceps used in conventional laparoscopic surgery. The robotic device using EndoWrist® function reported to be useful for suprapancreatic lymph node dissection, which is hard to accomplish with conventional laparoscopic technique (7).
Terashima et al. and Obama et al. (5,7) reported the number of lymph nodes retrieved in robotic surgery has been shown to have no significant differences compared to laparoscopic surgery. Therefore, robotic approach for the treatment of gastric cancer could be oncologically proper alternative to LG. However, Yonsei University reported that the number of dissected lymph nodes in the splenic artery and splenic hilum areas was significantly higher with robotic surgery in a study regarding D2 dissections (12). In a study comparing robotic total gastrectomy with D2 lymphadenectomy and laparoscopic total gastrectomy with D2 lymphadenectomy, Son et al. (12) reported that there were no differences in the number of retrieved lymph nodes (47.2 vs. 42.8, respectively) while the mean number of retrieved lymph nodes along the splenic artery and in the area of the splenic hilum was higher with robotic surgery than laparoscopic surgery. This result provides more sufficient dissection of the lymph nodes at the splenic hilum and along the splenic artery due to accurate and exquisite manipulation without tremors and that can be lead to more accurate staging and potential of improved long-term survival of patients with gastric cancer (7). Xiong et al. (13) conducted meta-analysis of nine non-randomized comparative studies with 2,495 patients (RG 736 and LG 1,759) reported that there was no significant difference in the number of retrieved lymph nodes. Another systemic review and meta-analysis of nine non-randomized observational clinical studies involving 7,200 patients conducted by Hyun et al. (2) described the number of retrieved lymph nodes in robotic surgery was comparable with that of laparoscopic surgery. Therefore, we can find that RG also provides an oncologically adequate lymphadenectomy.
Short-term outcomes
Postoperative complication
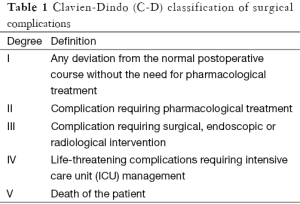
Avoiding postoperative complication is an important meaning of minimal invasiveness. When evaluating postoperative complications, previously validated complication grading systems such as the Clavien-Dindo (C-D) classification can be used and many studies examined here used that classification (Table 1) (2,6,8,10). It allows complications to be reported in an objective, simple, reliable, and reproducible manner based on the degree of therapy (10).
Full table
Terashima et al. (5) reported there was no difference between RG and LG on their study evaluated 18 cases with the incidence of intra-abdominal infectious complications. In addition, analysis of the frequency of postoperative complications revealed no differences between RG and LG. Seo et al. (14) evaluated the operative complications including the postoperative pancreatic fistula (POPF) with 40 gastric cancer patients who underwent robotic distal gastrectomy (RDG) and compared with 40 initial patients who underwent laparoscopic distal gastrectomy (LDG) by a single surgeon. They reported that POPF after distal gastrectomy was observed more frequently in the LG group than in the RG group (22.5% vs. 10%, P<0.001) and the serum amylase level was significantly lower in robotic surgery than in laparoscopic surgery (P<0.05). Consequently, the onset rate of pancreatic juice leakage was significantly lower in robotic surgery than in laparoscopic surgery. Seo et al. (14) also stated the possibility of reducing postoperative complications with robotic surgery in regard to reconstruction and exquisite procedures. RG may increase the ease of reconstruction and reduce postoperative complications in exquisite procedures, particularly peripancreatic lymph node dissection.
Uyama et al. (15) used their integrated robotic approach for performing suprapancreatic D2 nodal dissection in 25 patients with gastric cancer recently and compared short-term outcomes between RG and LG. There were no complications related to pancreatic damage in the RG group. Kim et al. (16) reported the study integrating the most cases is a single institutional retrospective comparative study of RG and LG. They compared postoperative complication rates, in 436 and 861 patients receiving RG and LG and there were no significant differences among groups regarding the overall complications. Recently, several meta-analyses comparing RG and LG and a few systematic reviews about RG suggest that overall complications are not significantly different (2,17-20). Study conducted by Son et al. (12), comparing RG with D2 lymphadenectomy and LG with D2 lymphadenectomy, reported that there were no differences in postoperative complication rate (16% vs. 22%, respectively). In another systematic review and meta-analysis, nine non-randomized observational clinical studies involving 7,200 patients were evaluated and post-operative complications were similar in two groups, robotic and laparoscopic (14).
Kim et al. (8) conducted multicenter prospective comparative study of RG and LG for gastric cancer. A total of 434 patients were enrolled for treatment with either robotic (n=223) or laparoscopic (n=211) gastrectomy for intention-to-treat analysis, and a total of 370 patients (n=185 per treatment) were compared in per-protocol analysis. In both intention-to-treat and per-protocol analyses, the rates of overall complications [11.9% (robotic) vs. 10.3% (laparoscopic); P=0.619] and major complications [1.1% (robotic) vs. 1.1% (laparoscopic); P>0.999] were similar between the two groups. Also, types of complications were comparable. Meta-analysis conducted by Maeso et al. (21) stated no significant difference between the surgical techniques in terms of the number of patients suffering some complication. Hyun et al. (2) reported that there were no differences in total postoperative complication rates, leakage rates and stenosis between RG and LG in all studies they analyzed. Hyun et al. (10) also analyzed 121 consecutive gastric cancer patients underwent gastrectomy (38 RG vs. 83 LG) from February 2009 to November 2010 at the Department of Surgery, Korea University Anam Hospital, Seoul, Korea and the C-D classification was used to grading surgical complications. Overall postoperative complications were more common in RG (47.3% vs. 38.5%), but the difference was not significant (P=0.361). Minor complications (C-D classification I and II) were more common in RG (34.1% vs. 21.6%; P=0.143). In contrast, major complications (C-D classification III and IV) were more common in LG (16.8%) than in RG (13.1%; P=0.603) patients.
Almost all reports have stated overall postoperative complications of RG are comparable to those of LG (2-5,8-10,21,22). But several reports mentioned potential of RG reducing postoperative complications, which can lead to further improvements in short-term outcomes, in that there were no complication regarding pancreatic damage in RG and significant improvements in local complications, such as pancreatic fistula formation, associated with sophisticated procedure (5,7).
Hospital stay
Hospital stay is an important outcome of RG and LG. In systematic review and meta-analysis of Hyun et al., the nine non-randomized observational clinical studies involving 7,200 patients satisfied the eligibility criteria, mean hospital stay for RG was similar to that for laparoscopic surgery (P=0.14) (2). And a multicenter prospective comparative study of et al. showed that length of hospital stay were similar between the two groups [6 (robotic) vs. 6 (laparoscopic) days; P=0.862] (8). Also, a prospective trial of Huang et al. showed that there was no significant difference in the postoperative hospital stays (11). Other studies also have similar results that are no significant difference of hospital day between RG and LG (4,10). In conclusion, the majority of current study shows that hospital day is similar between RG and LG.
Blood loss
About perioperative blood loss, there are recent meta-analyses comparing RG and LG. In meta-analysis made by systematic searching of all articles published between 1990 and 2011, Xiong et al. (23) showed significant reduction in blood loss when RG is used compared with LG. Also, Son et al. researched three meta-analyses that showed the same result for blood loss (1). However, a systematic review and meta-analysis by Maeso et al. revealed that no significant difference between RG and LG in the amount of blood loss (21). So, in blood loss, researchers have no definite consensus and have not found obvious difference between RG and LG yet. Also, there is an interesting idea by Son et al. that statistically significant difference is negligible unless the small amount of progress in blood loss reduction has a certain clinical or oncologic benefit (1). So not only an obvious difference of the amount of blood loss between RG and LG, but also the relationship between the amount of blood loss and oncologic benefit are the important factors that determine a value of blood loss as a perioperative outcome.
Conversion rate
If RG or LG is being performed, there is an inevitable situation that the procedure might convert to an open gastrectomy. High conversion rates can lead to unsatisfactory consequences. Theoretically, RG has a tent effect (camera arm and endoscope lift up the abdominal wall) without laparoscopic gas procedure. So in cases of hypercapnia, the ‘‘tent effect’’ provides good vision even with low pressure of pneumoperitoneum, thereby reducing the probability of an open conversion compared with LG (9). However, a few number of cases of RG and LG were converted to open gastrectomy by many researches. A multicenter prospective comparative study conducted by Kim et al. revealed two open conversions in RG and one open conversion in LG (8). So statically, there is no difference between RG and LG, but case number is too small to have clinical meaning. A systematic review by Coratti et al. revealed no particular differences in conversion rates between RG and LG. Some reports showed results in favor of RG, still others favored LG, but there is no significant statistical difference (9). Consequently, it seems that a conversion rate has no significant difference.
Long-term outcomes
The da Vinci surgical system which is used in RG is approved by the Food and Drug Administration (FDA) in 2000. This novel system has a learning curve. So the history of RG which conducted by experienced operators is not long enough and sufficient for researching long-term outcomes. However, despite short history, there are some analyses for long-term outcomes.
In a non-randomized study compared RG and LG, Pugliese et al. (24), reported that the overall 3-year survival was 85% for LG and 78% for RG, but there is no statistically significant difference [the log rank test (P>0.05)]. Also, in the study of spleen-preserving RG compared with LG, Son et al. (12), reported that overall and disease-free survival between two groups were not significantly different (P=0.767 and P=0.666).
However, the majority of review articles reported commonly that the problem of study results to date is absence of randomized-controlled trial of long-term outcomes, such as recurrence rates or mortality of RG compared with LG. So in many research, the prediction of long-term outcomes is conducted by using various short-term outcomes (10,11). Consequently, there is no randomized-controlled trial and only prediction by short-term outcomes, so it can’t be concluded that which one is superior in terms of long-term outcomes at the current status.
Cost
The higher cost of RG is the main disadvantage. The principal reason for the higher RG-associated cost is the cost of the robotic system itself, and the depreciation reserve (1). Huang et al. reported that mean medical cost of RG is US $1,472 more expensive than mean medical cost of LG, and this difference is statistically significant (P<0.001).
However, each country has a different health insurance system. So the analysis in Korea might be important. Kim et al. reported that patients in RG accrued significantly higher total costs than patient in LG [\13,748,422.5 (RG) vs. \9,165,862 (LG); P<0.001]. Also, the cost covered by the Korean National Health Insurance for the robotic group was significantly less than that covered for the laparoscopic group. Consequently, the actual cost that patients paid is leaving significantly higher to patients in RG (\11,622,210) than LG (\4,145,050) (8). In other study, Park et al. reported that the significant difference of total cost between RG and LG is €3,189 and self-reported satisfaction level was significant higher in LG than RG (P=0.031) (25). Consequently, RG is higher cost than LG at the current status.
Conclusions
There are many uncertain and controversial issues comparing RG with LG and they are discussed thoroughly to handle a clear conclusion. Some points in this paper may be helpful for determining the advantages of RG compared with LG.
Shorter learning curve is an advantage of RG, but there is limitation that most results are conducted by highly professional laparoscopic gastric surgeons.
Lymph node yield of RG is comparable to LG. Almost all studies reported no significant differences have been observed regarding the number of dissected lymph nodes retrieved between RG group and LG group. This means RG provides more sufficient lymphadenectomy than LG in the area of the splenic hilum and that can lead to reductions in local complication rates and survival benefit regarding accurate D2 lymph node dissection.
Short-term outcomes such as postoperative complication, hospital day, blood loss, conversion rates may not be favorable results for both RG and LG. Except blood loss, there are no significant differences between RG and LG in short-term outcomes. Although blood loss is less in RG, the amount of the difference is not uniform and there is no consensus about whether that difference has clinical importance. About postoperative complication, almost all reports have stated that overall postoperative complications of RG are comparable to those of LG. Furthermore, conversion rates and hospital day have no significant difference also. Consequently, Short-term outcomes reported up to date may not verify the superiority of RG compared to LG.
Long-term outcomes are the most important factors for comparing RG to LG. However, research concerning long-term follow-up is still insufficient because of short history of RG. Therefore, it is difficult to evaluate the oncological efficacy of RG pertaining to recurrence and survival.
Cost is a definite disadvantage of RG and is significantly higher than LG.
Therefore, a well-designed randomized controlled trial is needed before coming to conclusion regarding long-term outcomes, recurrence and survival rate.
Acknowledgements
This work was supported by the Industrial Strategic Technology Development Program (10051331) funded by the Ministry of Trade, Industry and Energy (MOTIE) of Korea.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Son T, Hyung WJ. Robotic gastrectomy for gastric cancer. J Surg Oncol 2015;112:271-8. [PubMed]
- Hyun MH, Lee CH, Kim HJ, et al. Systematic review and meta-analysis of robotic surgery compared with conventional laparoscopic and open resections for gastric carcinoma. Br J Surg 2013;100:1566-78. [PubMed]
- Köckerling F. Robotic vs. Standard Laparoscopic Technique - What is Better? Front Surg 2014;1:15. [PubMed]
- Kang BH, Xuan Y, Hur H, et al. Comparison of Surgical Outcomes between Robotic and Laparoscopic Gastrectomy for Gastric Cancer: The Learning Curve of Robotic Surgery. J Gastric Cancer 2012;12:156-63. [PubMed]
- Terashima M, Tokunaga M, Tanizawa Y, et al. Robotic surgery for gastric cancer. Gastric Cancer 2015;18:449-57. [PubMed]
- Nishimura K. Current status of robotic surgery in Japan. Korean J Urol 2015;56:170-8. [PubMed]
- Obama K, Sakai Y. Current status of robotic gastrectomy for gastric cancer. Surg Today 2015. [Epub ahead of print]. [PubMed]
- Kim HI, Han SU, Yang HK, et al. Multicenter Prospective Comparative Study of Robotic Versus Laparoscopic Gastrectomy for Gastric Adenocarcinoma. Ann Surg 2015. [Epub ahead of print]. [PubMed]
- Coratti A, Annecchiarico M, Di Marino M, et al. Robot-assisted gastrectomy for gastric cancer: current status and technical considerations. World J Surg 2013;37:2771-81. [PubMed]
- Hyun MH, Lee CH, Kwon YJ, et al. Robot versus laparoscopic gastrectomy for cancer by an experienced surgeon: comparisons of surgery, complications, and surgical stress. Ann Surg Oncol 2013;20:1258-65. [PubMed]
- Huang KH, Lan YT, Fang WL, et al. Comparison of the operative outcomes and learning curves between laparoscopic and robotic gastrectomy for gastric cancer. PLoS One 2014;9:e111499. [PubMed]
- Son T, Lee JH, Kim YM, et al. Robotic spleen-preserving total gastrectomy for gastric cancer: comparison with conventional laparoscopic procedure. Surg Endosc 2014;28:2606-15. [PubMed]
- Xiong J, Nunes QM, Tan C, et al. Comparison of short-term clinical outcomes between robotic and laparoscopic gastrectomy for gastric cancer: a meta-analysis of 2495 patients. J Laparoendosc Adv Surg Tech A 2013;23:965-76. [PubMed]
- Seo HS, Shim JH, Jeon HM, et al. Postoperative pancreatic fistula after robot distal gastrectomy. J Surg Res 2015;194:361-6. [PubMed]
- Uyama I, Kanaya S, Ishida Y, et al. Novel integrated robotic approach for suprapancreatic D2 nodal dissection for treating gastric cancer: technique and initial experience. World J Surg 2012;36:331-7. [PubMed]
- Kim KM, An JY, Kim HI, et al. Major early complications following open, laparoscopic and robotic gastrectomy. Br J Surg 2012;99:1681-7. [PubMed]
- Liao G, Chen J, Ren C, et al. Robotic versus open gastrectomy for gastric cancer: a meta-analysis. PLoS One 2013;8:e81946. [PubMed]
- Shen WS, Xi HQ, Chen L, et al. A meta-analysis of robotic versus laparoscopic gastrectomy for gastric cancer. Surg Endosc 2014;28:2795-802. [PubMed]
- Baek SJ, Kim SH. Robotics in general surgery: an evidence-based review. Asian J Endosc Surg 2014;7:117-23. [PubMed]
- Marano A, Hyung WJ. Robotic gastrectomy: the current state of the art. J Gastric Cancer 2012;12:63-72. [PubMed]
- Maeso S, Reza M, Mayol JA, et al. Efficacy of the Da Vinci surgical system in abdominal surgery compared with that of laparoscopy: a systematic review and meta-analysis. Ann Surg 2010;252:254-62. [PubMed]
- Güner A, Hyung WJ. Minimally invasive surgery for gastric cancer. Ulus Cerrahi Derg 2013;30:1-9. [PubMed]
- Xiong B, Ma L, Zhang C. Robotic versus laparoscopic gastrectomy for gastric cancer: a meta-analysis of short outcomes. Surg Oncol 2012;21:274-80. [PubMed]
- Pugliese R, Maggioni D, Sansonna F, et al. Subtotal gastrectomy with D2 dissection by minimally invasive surgery for distal adenocarcinoma of the stomach: results and 5-year survival. Surg Endosc 2010;24:2594-602. [PubMed]
- Park JY, Jo MJ, Nam BH, et al. Surgical stress after robot-assisted distal gastrectomy and its economic implications. Br J Surg 2012;99:1554-61. [PubMed]


